August 10, 2020 Important of Wearing a Mask
July 15, 2020
Officials in Houston are warning that the situation could become a replay of what happened in New York City in March and April, when thousands of people died as hospitals struggled to keep up with the surge of patients, but without the same level of government intervention to stem the tide.
Typically when people arrive at a hospital emergency department, they’re evaluated and treated by the medical staff. Those sick or injured enough to require hospitalization are then moved to other areas of the hospital for specialized care. But increasingly in Houston, particularly for patients suffering from COVID-19, there’s nowhere for them to go.
“Normally that patient would just go to an ICU bed, but because there are no beds available, they continue to board in the emergency room,” said Harris Health System president and CEO Esmaeil Porsa, who oversees the city’s two public safety-net hospitals. “It is not an optimal level of care. This is not something we would choose to do. The only reason this is happening is because we are being forced to do it.”
Although hospital leaders say they are working to provide high-quality care for patients being held in emergency rooms — in part by bringing specialized medical staff and equipment to patients being treated there — studies done before the coronavirus pandemic show that the longer patients stay in ERs, the worse their outcomes.
ICUs and other hospital units are staffed with doctors, nurses and other support personnel who have specialized training and experience caring for critically ill patients in need of specific medical interventions, whereas the mission of emergency department medical workers is to quickly assess patients, stabilize them and get them to where they need to be.
“The problem is you can’t get them to where they need to be, and now it puts the ER doc in the position of having to function like the hospitalist or the intensive care doctor, and that’s not a role that we’re really supposed to be in,” said Dr. Cedric Dark, an emergency physician at Baylor College of Medicine in Houston. “The bad thing about having any patient boarded in the emergency department, regardless of the situation, is that it slows down the beginning of care for somebody who needs hospitalization, and the beginning of care for any medical condition is the most crucial period of time.”
The same scenario is playing out at hospitals across the Houston region.
A daily status report prepared Wednesday by the SouthEast Texas Regional Advisory Council, which coordinates the Houston region’s emergency medical response, showed multiple hospitals running out of immediately available nonsurgical ICU beds, including both of the city’s top-tier trauma centers, Ben Taub Hospital and Memorial Hermann’s flagship hospital in the Texas Medical Center.
As of Wednesday afternoon, about 145 patients were being held in emergency departments throughout the Memorial Hermann Health System, according to internal numbers provided separately by a Memorial Hermann physician and confirmed by a hospital executive. Several other Houston area hospitals have reported holding multiple patients in their ERs, including four with more than a dozen.
Get Our Top Investigations
Subscribe to the Big Story newsletter. Email address This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Dr. Jamie McCarthy, an executive vice president at Memorial Hermann Health System and an emergency room physician, acknowledged that the coronavirus crisis has forced his teams to hold more patients in ERs.
“All the hospitals are full,” McCarthy said. “All the hospitals in the city are boarding patients. We are expanding capacity, but we can’t turn those on immediately. It requires staffing. It requires nurses and doctors to come in. And so, as we’ve continued to expand our inpatient capacity, we’re just keeping up with the volume that’s coming in.”
It’s not unusual for a small number of patients to be held in ERs on busy days, especially during flu season, but three Houston ER physicians said they have never seen so many patients receiving prolonged care in emergency departments, or for such long periods of time.
Although treating patients in the ER for more than a few hours is “not ideal,” McCarthy said, Memorial Hermann has worked to mitigate the impact on patients by sending intensive care doctors and other specialists to emergency departments, to ensure patients are receiving quality care regardless of where they’re located.
But he warned that there’s a limit to what Houston hospitals can do to respond to the crisis.
Read More
Andrew Cuomo’s Report on Controversial Nursing Home Policy for COVID Patients Prompts More Controversy
A state report on Cuomo’s decision to order nursing homes to take in COVID positive patients in the early days of the pandemic fails to deal with the central question: did such admissions lead to more infection and death, and if so how significantly.
“We are adding more capacity, but we are absolutely stretched now, and if it keeps going this way, we’re going to run out of room. We’re going to look like New York,” McCarthy said, emphasizing the need for Houston residents to stay home and avoid crowds to slow the virus’s spread.
One of Houston’s largest hospital systems, HCA Healthcare, also has been caring for dozens of COVID-19 patients in its emergency departments. In a statement, HCA spokeswoman Debra Burbridge said hospital officials have taken steps to reduce the impact on patients, including sending staff members who would normally be performing or assisting with elective surgeries — which have been suspended under an order by the governor — to treat patients with COVID-19.
Dr. Kusum Mathews, an assistant professor of critical care and emergency medicine at the Icahn School of Medicine at Mount Sinai in New York, said hospitals can take steps to reduce the risks of overcrowded ERs, including some of those described by Memorial Hermann and HCA officials.
Treating patients sickened by the virus “has outstripped every stretch of our imagination,” Mathews said. “We have had to put beds in hallways, double up patient rooms … just to allow for offloading the emergency department to get more patients in.”
While Houston’s top hospital executives have repeatedly said they can add hundreds of new intensive care beds to meet the demand, at least for the next couple of weeks, the number of patients being treated in emergency rooms demonstrates the difficulty of executing those plans in the midst of a rapidly growing crisis, officials say.
“Those things are not like a switch-key type of activity,” said Porsa, the Harris Health System CEO, noting that his hospitals have had to send patients to hospitals outside of Houston to make room. “The bottleneck to do that is really staffing. As you can imagine, ICU nurses are not a dime a dozen. They are very hard to come by, and it takes time to actually be able to do that.”
The logjam of patients being treated in ERs has also led to delayed emergency response times across the city, according to Houston Fire Department officials.
When hospitals get overloaded, they ask regional authorities to divert ambulances elsewhere. For example, Memorial Hermann’s northeast hospital was on diversion status just 2% of the time during an eight-day period in late June and early July last year; it was on diversion status 58% of the time during the same time period this year. At Houston’s busiest public hospital, Ben Taub, the number jumped to 81% from 58%.
The problem, said Houston Fire Department Assistant Chief Matt White, is that when every hospital is maxed out, ambulance crews have no choice but to take patients to emergency departments that are too busy to quickly receive them. And by law, hospitals must screen and stabilize any patient who arrives.
“When everyone is on diversion,” White said, “nobody is on diversion.”
Earlier coronavirus outbreaks inundated emergency rooms in New York City and Detroit, but lockdown orders in those cities led to fewer car accidents and a reduction in violent crime, freeing more space in ERs for COVID patients.
Read More
Three Takeaways From the Supreme Court’s Decisions on Trump’s Tax and Financial Documents
The Supreme Court finally ruled on whether Congress and investigators can obtain the president’s financial information. The answer is yes — but it’s a little more complicated than that.
With most Texas businesses still open and no mandatory stay-at-home order, hospitals in Houston and other COVID-19 hot spots face the added challenge of making room for COVID patients while still dealing with a steady flow of patients seeking care for other medical emergencies.
And across the country, people with chronic health problems who delayed seeking care earlier in the pandemic are now showing up for treatment, taking up beds, said Dr. Marc Eckstein, medical director of the Los Angeles Fire Department and a professor of emergency medicine at Keck School of Medicine of the University of Southern California.
Despite these challenges, McCarthy, the Memorial Hermann executive, said it’s essential that people continue to come to the hospital for medical emergencies. He pointed to an NBC News and ProPublica report this week that showed a growing number of people are dying suddenly at home, before emergency responders can reach them.
“If a patient believes they have a serious medical issue, they still need to come to the emergency department,” McCarthy said. “We will make the capacity to take care of them. Delaying care for time-sensitive emergencies is time we don’t get back. If they wait to call for help when they are having a heart attack, it will be worse than if they come in early.”
7/14/2020
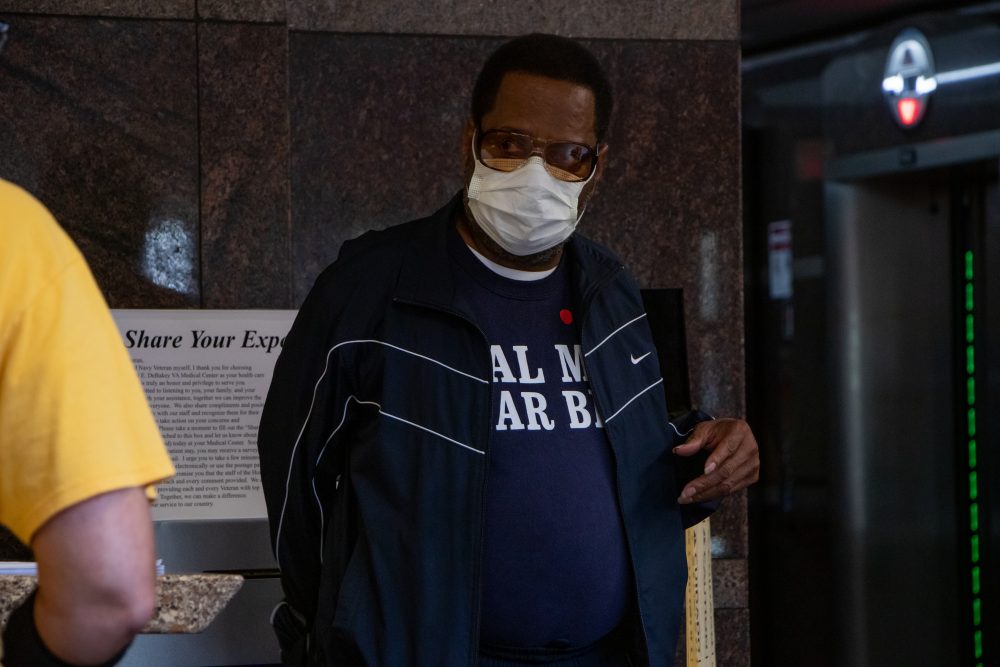
How Effective are Face Masks versus Face Shields
7/2/2020: UPDATE – FDA warns consumers of risk of methanol contamination in certain hand sanitizers
FDA is warning consumers and health care providers that the agency has seen a sharp increase in hand sanitizer products that are labeled to contain ethanol (also known as ethyl alcohol) but that have tested positive for methanol contamination. Methanol, or wood alcohol, is a substance that can be toxic when absorbed through the skin or ingested and can be life-threatening when ingested.
The agency is aware of adults and children ingesting hand sanitizer products contaminated with methanol that has led to recent adverse events including blindness, hospitalizations and death.
Methanol is not an acceptable active ingredient for hand sanitizers and must not be used due to its toxic effects. FDA’s investigation of methanol in certain hand sanitizers is ongoing. The agency will provide additional information as it becomes available.
Consumers who have been exposed to hand sanitizer containing methanol and are experiencing symptoms should seek immediate treatment for potential reversal of toxic effects of methanol poisoning. Substantial methanol exposure can result in nausea, vomiting, headache, blurred vision, permanent blindness, seizures, coma, permanent damage to the nervous system or death. Although all persons using these products on their hands are at risk for methanol poisoning, young children who accidently ingest these products and adolescents and adults who drink these products as an alcohol (ethanol) substitute, are most at risk.
FDA reminds consumers to wash their hands often with soap and water for at least 20 seconds, especially after going to the bathroom; before eating; and after coughing, sneezing, or blowing one’s nose. If soap and water are not readily available, the Centers for Disease Control and Prevention (CDC) recommend consumers use an alcohol-based hand sanitizer that contains at least 60 percent ethanol (also referred to as ethyl alcohol).
FDA remains vigilant and will continue to take action when quality issues arise with hand sanitizers. The agency is especially concerned with:
- The dangers of drinking any hand sanitizer under any conditions. While hand sanitizers with possible methanol contamination are more life-threatening than those that are not contaminated, FDA urges consumers not to drink any of these products.
- Certain hand sanitizers that may not contain a sufficient amount of ethyl alcohol or isopropyl alcohol.
- Hand sanitizers that are sold or offered for sale with false and misleading, unproven claims that they can prevent the spread of viruses such as COVID-19, including claims that they can provide prolonged protection (e.g., for up to 24-hours).
- Products that are fraudulently marketed as “FDA-approved” since there are no hand sanitizers approved by FDA.
- Products packaged to appear as drinks, candy or liquor bottles, as well as products marketed as drinks or cocktails because their appearance could result in accidental ingestion or encourage ingestion. Children are particularly at risk with these products since ingesting only a small amount of hand sanitizer may be lethal in a young child.
FDA is aware of reports of adverse events associated with hand sanitizer products. FDA encourages health care professionals, consumers and patients to report adverse events or quality problems experienced with the use of hand sanitizers to FDA’s MedWatch Adverse Event Reporting program (please provide the agency with as much information as possible to identify the product):
- Complete and submit the report online; or
- Download and complete the form, then submit it via fax at 1-800-FDA-0178.
A Message from the Texas Medical Center
Texas Governor Urges Residents to Stay Home Amid Record Number of Corona Virus Cases
Texas Gov. Greg Abbott (R) is imploring residents to stay home as the state grapples with a surge in coronavirus cases and hospitalizations stemming from the disease.
In an interview Tuesday with local CBS affiliate KBTX-TV, Abbott said Texas would report more than 5,000 cases of COVID-19 from the previous 24-hour period, marking a new high in the state. He added that hospitalizations were also at an all-time high, stressing that the outbreak is “serious.”
“First, we want to make sure that everyone reinforces the best safe practices of wearing a mask, hand sanitization, maintaining safe distance, but importantly, because the spread is so rampant right now, there’s never a reason for you to have to leave your home,” Abbott said. “Unless you do need to go out, the safest place for you is at your home.”
Abbott noted that more announcements regarding the state’s efforts to combat the spread of the disease would come later in the week. He said that the state has increased testing and response supplies in areas being hit especially hard by outbreaks. He also said that the Texas Alcoholic Beverage Commission has expanded enforcement efforts to ensure businesses are complying with health restrictions.
But the governor said during a press conference on Monday that he would not reimpose any restrictions on businesses and other activities. While admitting that the increase in cases was “unacceptable,” he said that the state would remain “open for business.”
“We don’t have to choose between jobs and health. We can have both. We can protect Texan lives while also restoring livelihoods. … Together, we will keep Texas wide open for business,” he said, urging Texans to wear masks, wash their hands and maintain social distancing.
The governor stopped short of announcing any new restrictions to curb the spread of the disease.
“Closing down Texas again will always be the last option,” Abbott said.
Texas was one of the first states to begin a gradual reopening in late April. The state is now on the third phase of that reopening, which allows businesses, including bars, gyms and office buildings, to operate at 50 percent capacity. Some businesses have also been permitted to operate at 100 percent capacity, and few restrictions are in place for most outdoor areas.
As of Tuesday, state health officials had reported more than 120,000 COVID-19 cases and more than 2,200 deaths caused by it. The Texas Department of State Health Services said in a statement Monday that “hospitalizations are rising at their fastest rate yet.”
Abbott told KBTX-TV that the “first obligation we have is to make sure people around the state really comprehend the magnitude of the challenge we’re dealing with.”
“There remain a lot of people in the state of Texas who think that the spread of COVID-19 is really not a challenge,” he said.
Gov. Abbott Allows Restrictions on Gatherings Over 100 People
https://abc13.com/covid-abbott-gatherings-social-distancing/6262723/
Judge Signs Order for Masks in Ft. Bend County
RICHMOND (Covering Katy News) – Fort Bend County Judge K.P. George has signed an order to make all businesses require that employees and customers wear face coverings. The new order goes into effect at midnight on June 25.
George said 77.5% percent of people who responded to a recent survey were in favor of requiring masks.
“Maybe we are tired of COVID, but it looks like COVID is not tired of us. It’s around here,” Fort Bend County Judge KP George said during a briefing. “It is about helping our community recover and helping our community combat this unprecedented time,” said George.
June 16, 2020
What Makes an RNA Vaccine Different From a Conventional Vaccine
June 16, 2020
Gas Stations (and Your Car) Are Germ City—Here’s How to Stay Safe and Clean on the Road
Getty Images
What if we told you your steering wheel might be harboring more germs than a toilet seat, or that the average gas station pump handle is—wait for it—6,428 times dirtier than public elevator buttons?
Help.
Whether you’re popping downtown to fill up on groceries and gas, or headed out on a family road trip, you’re going to want to maintain a clean car and smart hygiene habits between point A and point B. Think about it. You’ve been keeping your home (and self) spick and span since the coronavirus outbreak—disinfecting surfaces, washing hands thoroughly, wearing a mask in public, and practicing social distancing. So now that parts of the country are opening up and the urge to take a joy ride is becoming harder to resist, it’s time to bring all those responsible practices with you on the road, too.
RELATED: 7 Things You Should Sanitize Immediately to Avoid Getting Sick
Exactly how germy is your car?
The concept of deep-cleaning the interior of your car—not just giving the exterior a good shine—goes way beyond protecting from the coronavirus. In general, cars are insanely dirty, harboring, on average, somewhere around 700 bacterial strains, including staphylococcus (though, remember, many bacteria are relatively harmless).
In a recent survey of 1,000 drivers, CarRentals.com reported that, despite the griminess of most vehicles, 32 percent of drivers only clean their cars once a year. What’s more, 20 percent regularly eat in the car (and who hasn’t?). But what might seem like harmless road trip snacking can be potentially harmful: spilled food and drinks + time and a stuffy car = bacteria heaven.
CarRentals.com also did some research to find the average number of colony-forming units (CFU)—aka the amount of bacteria per square centimeter—on cars’ most commonly touched surfaces and compared those to the CFU count on other public surfaces. Ready to cringe?
The average steering wheel was found to have 629 CFU per square centimeter, which is:
- Six times dirtier than an average cell phone screen (100 CFU)
- Four times dirtier than a public toilet seat (172 CFU
- Two times dirtier than public elevator buttons at (CFU)
Some of the other germiest spots in the average vehicle, according to these findings, include commonly touched surfaces like the cupholders (506 CFU), seatbelt (403 CFU), interior door handles (256 CFU), gear shift (115 CFU), and audio volume (99).
Let’s just say that’s the last time we’ll be eating french fries off the dashboard.
RELATED: 7 Common Hand-Washing Mistakes to Avoid
Gas stations are germ-central.
Pumping gas is routine for any driver, but we all need to be smart about it. Don’t forget how many other people have used those buttons, handles, and other touch points before you (likely thousands). Clocking in at an eye-popping 2 million CFU of germs, the average gas pump handle was found to be 6,428 times dirtier than public elevator buttons and 11,835 times dirtier than a public toilet seat. But dirtier still, the button for regular, unleaded gas takes the cake in this analysis with 3.2 million CFU, compared to the premium buttons with 2 million CFU.
RELATED: Don’t Know the Difference Between Sanitizing and Disinfecting? You Might Not Be Cleaning Properly
Stay safe on the road, at gas stations and everywhere in between.
If you’re certifiably freaked out at the moment, take a pause. Remember that gas stations (and your car) have always been dirty—long before the virus outbreak and long before you read all these stats. You’ve been driving and pumping gas and living to tell the tale for years. Just consider this a wakeup call to adopt some sanitation best practices on the road, just in case. To get started, read these engineer-approved car-cleaning tips from Ford, plus some input from Beaumont Hospital Infection Prevention in Michigan on how to stay safe at gas stations, roadside rest stops, and other mid-drive destinations.
1. Have hand sanitizer at the ready.
The pocket of your door panel, center console, or even a bag/purse are smart locations for hand sanitizer (make sure it has at least 60 percent alcohol content). Clean your hands with it every time you’re done at the store, restaurant, or gas station.
Can’t find any at the store? Here’s how to make your own hand sanitizer. Avoid touching your face as much as possible, but especially before disinfecting your hands post-pump.
2. Keep sanitizing wipes handy, too.
Give these major touch points a sanitizing swipe every time you get in the car: the steering wheel, temp control knobs, gear shifter, touch screen, door handles (inside and out), arm rests, and cup holders.
3. Store a clean face mask or two in the car.
Keep a couple clean cloth face masks over your sun visor so you have one handy for unexpected errands or pit stops, whether to the grocery store or a rest stop restroom.
RELATED: Need a Cloth Face Mask? Here’s Where to Buy Them Right Now
4. Use disposable gloves to pump your gas.
Ford experts suggest wearing gloves for touching gas pump handles and car wash wands. But doing so is pointless unless you remove and dispose of them properly directly afterwards using to avoid contamination. Take extra precaution by sanitizing hands afterward.
5. Keep payments as clean as possible.
The stuff in our wallets—and in cash registers—is, well, gross, to put it plainly. Cash is notoriously dirty, while credit and debit cards are shockingly germ-infested in their own right. (But good news, you can clean your credit cards safely!). Ford and Beaumont agree that if you have to use cash, try your best to give exact change to avoid a contaminated money swap. “Or tell them to keep the change,” Ford says. “Better yet, use an app to order and pay in advance,” if you’re stopping at a fast food joint, for instance.
6. Deep-clean the interior.
At the end of a longer road trip—or even if it’s just been awhile—give the interior of your car a solid sudsing. Use a sanitizing wipe to clean the seats, gear shift, steering wheel, and door handles. CarRentals.com says to replace the air filter and spray into the intake vent to remove airborne germs in the carbon cabin. Wash the seats with car upholstery shampoo and clean or replace the floor mats. And don’t forget to disinfect your keys! This handheld accessory is just begging to be cleaned on the regular.
For more car cleaning tips, roll up your sleeves and follow this guide to deep-cleaning your car routinely.
Houston on ‘Precipice of Disaster’ With Virus Cases Spreading
Houston-area officials are “getting close” to reimposing stay-at-home orders and are prepared to reopen a Covid-19 hospital established but never used at a football stadium as virus cases expand in the fourth-largest U.S. city.
The announcement by Harris County Judge Lina Hidalgo and Houston Mayor Sylvester Turner on Thursday came a day after the Lone Star state recorded its highest one-day tally of new cases since the pandemic emerged.
Read More: Second U.S. Virus Wave Emerges as Cases Top 2 Million
“We may be approaching the precipice of a disaster,” said Hidalgo, the highest-ranking county executive. “It’s out of hand right now. The good news is it’s not severe out of hand.”
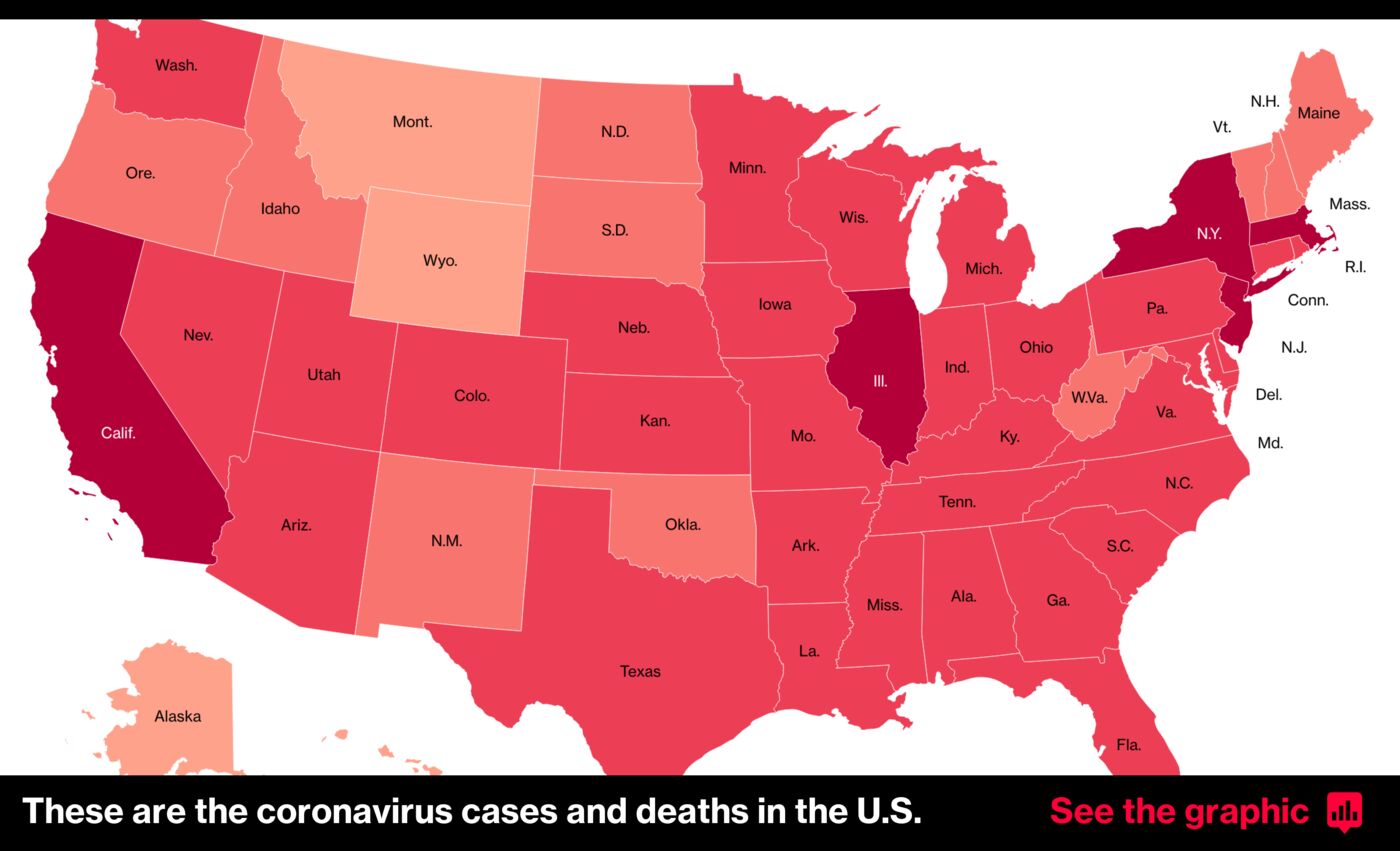
The warnings of a worsening outbreak reinforced alarms sounded by national health officials over the risk of a second wave of infections beyond the initial U.S. hot spots led by New York and New Jersey. Texas has been among the states pushing hardest to ease lockdowns imposed during the first wave of a disease that has killed more than 113,000 Americans.
However, any plan to reinstate local lockdowns may hold little legal authority after Governor Greg Abbott issued executive orders to reopen the state that superceded county and municipal directives, Hidalgo’s spokesman, Rafael Lemaitre, said in an email.
“Hidalgo believes the state is moving too fast to reopen,” Lemaitre wrote just hours after the announcement.
Death Toll
Harris County, which encompasses Houston and adjacent suburbs, has recorded 15,552 cases, almost one-fifth of the 81,583 statewide total, according to state health department data released Thursday.
Fatalities, however, remain small compared to so-called hot spots in other parts of the U.S. Harris County’s cumulative death toll of 267 is only about a third of what New York state was amassing each day during the darkest period of the outbreak.
In Texas, conditions are actually worse in Dallas County, a jurisdiction with 2 million fewer residents than Harris County that’s had 2.6% more deaths, according to the state health department figures.
Stadium Hospital
President Donald Trump visited Dallas on Thursday for a meeting with religious leaders, business owners and law enforcement officials before attending a fundraiser.
Harris County also instituted what it called a public health threat level assessment that will alert residents if conditions worsen or improve. The level remains at the second-highest on the four-tier scale.
The ad hoc medical facility opened at NRG Stadium on the city’s south side will be reestablished if pressure on the local hospital system becomes “severe,” Hidalgo said in a meeting with reporters.
“We’re moving in the wrong direction with hospital admissions and if it continues we’ll have to see what else we could do including sounding the alarm to our residents and moving our alert system to red,” Lemaitre wrote.
June 11, 2020
Texas Shatters Record For New Coronavirus Cases
TOPLINE
Texas reported over 2,500 new coronavirus cases Wednesday—the highest reported in a single day by far since the pandemic started—as the number of Texans currently admitted to hospitals for coronavirus climbed to a new record for the third straight day, as the state, which had one of the fastest and most aggressive reopening timelines in the nation, has seen a surge in infections about two weeks after Memorial Day.

KEY FACTS
The 2,504 cases reported by the Texas Department of Health Wednesday is more than 28% higher than any other day since the pandemic began, far surpassing the old record of 1,949 on May 31.
According to the Texas Department of Health, there were 2,153 patients hospitalized with coronavirus on Wednesday, surpassing records set each of the past two days and well ahead of the old record of 1,888 recorded on May 5.
The positive test rate, which state officials have used as a key figure in moving forward with reopening, has also gradually risen over the past two weeks.
The 7-day average for tests coming back positive reached its highest rate since mid-April this week, and is now above 6%—a threshold public health officials there have said they’d like the state to remain below.
Texas entered Phase 3 of its reopening last week, and restaurants will be able to operate at 75% capacity starting Friday, as the state continues its aggressive reopening while seeming to ignore White House guidance that says states need to see a downward trend either in new cases or the infection rate to move forward with reopening efforts.
Texas Gov. Greg Abbott has said several times in the past that the state should expect to see an increase in infections as testing ramps up, but that would not explain why there’s been a rise in hospitalizations or the percentage of tests coming back positive.
CRITICAL QUOTE
“In terms of new infections, we are seeing a surge … in part attributed to activities surrounding Memorial Day weekend, such as gatherings where protective behaviors may have been lax,” Rebecca Fischer, an epidemiologist at the Texas A&M School of Public Health, told the Texas Tribune.
KEY BACKGROUND
Texas isn’t alone in seeing cases jump over the past few days. Over a dozen states across the U.S., including California, have also had a concerning rise. Abbott has said in the past that if the state appeared to be going in the wrong direction, there might be some delay to reopenings, but that doesn’t seem to be the case so far with the rise in hospitalizations. A spokesman for the governor told the Texas Tribune that the state is far from a health capacity crisis, saying“every Texan who needs access to a hospital bed will have access to a hospital bed.”
New cases in the state have gone up sharply, though, with the 7-day average for new cases rising from under 1,000 new cases reported per day in late May to now over 1,500 cases per day. The number of deaths from coronavirus in the state has been relatively stable since mid-May, staying in the low- to mid-20s per day.
BIG NUMBER
42%—That’s about how much hospitalizations have increased in Texas since Memorial Day.

I’m a New Orleans-based news reporter for Forbes covering the U.S. South and breaking news. Previously, I wrote for The Times-Picayune | The New Orleans Advocate covering…
June 10, 2020
Banned From Nursing Homes, Families See Shocking Decline In Their Loved Ones
It wasn’t candlelight and soft music that made the 40th anniversary of Luann and Jeff Thibodeau so memorable. It was gazing at each other through the window of Jeff’s nursing home in Texas and eating carryout from the Olive Garden. Just the two of them. And a nursing assistant.
“She fed him, and I ate mine, and that was it,” Luann Thibodeau says. “So that was our 40th wedding anniversary.”
The Thibodeaus have not been in the same room since mid-March. That’s when visitors were banned from nursing homes to slow the spread of the coronavirus. But family members say that talking via FaceTime and holding up signs at windows are no substitute for the hands-on care and emotional support their visits provide.
Family members often are an integral part of the care residents in nursing homes receive. They make sure meals are being eaten, clothes are being changed. They also offer invaluable emotional support.
Without it, the consequences can be dire. NPR spoke to several families about what’s happened since the mid-March visitor ban. All reported seeing shocking declines in their loved ones.
Advocates for residents say it’s time to rethink the outright ban.
Nursing homes can permit visitors for “compassionate situations.” But that’s usually interpreted as meaning end-of-life visits. Robyn Grant, public policy director for the National Consumer Voice for Quality Long-Term Care, says that compassionate care needs to be interpreted more broadly.
“Residents are declining mentally, physically,” she says. “We think that those situations are times when family members should be permitted.”
Luann Thibodeau has seen that decline in her husband. She used to bring dinner for him every night except Tuesdays when she goes to Bible Study. She says that as his multiple sclerosis has worsened, he’s become increasingly disinterested in food.
“I bully him into finishing a meal. And I’ll say to him, ‘Jeff, you know, this is what an adult man eats. So you need to eat this.’ “
A staff member can’t do what she does. Nursing home residents have rights. So if Jeff Thibodeau tells a nursing assistant that he’s done eating after three bites, she has to abide by his wishes.
Without his wife’s push, the results of her absence is striking.
“When I see him at the window, I can tell his clothes are way big on him,” Luann Thibodeau says. “And I’m pretty sure he’s lost significant weight.”
And while family members are locked out, residents are locked in. It didn’t used to be like that. Luann Thibodeau would take her husband to church on Sundays and to the movies. They’d go out for fast food. But she says since the lockdown, his anxiety has increased. Sometimes he’s called her 10 times in a day.
“He would say, ‘Why aren’t you here? Why don’t you come in? Nobody will know,’ ” Luann Thibodeau says. “And he was strategizing how I could sneak in the front door. I could sneak in the back door and come see him. And so that’s been really hard.”
It’s also been really hard for Eva Gonzalez, a 98-year-old resident of a Southern California nursing home. She was used to daily visits from her sons Sky and David.
“She probably feels that we’ve abandoned her,” Sky Gonzalez says.
Eva Gonzalez lived on her own until about 18 months ago. Then she started having falls and symptoms of dementia. She needed 24-hour care. But now that Sky can only reach her on the phone, he can’t see what kind of care she’s getting.
“When I call, she always seems to be dehydrated,” he says.
She tells him she needs water. Nursing home staffers tell him they check on her every hour. “But how do I know what’s going on or not going on?” he asks.
Yet calling his mom directly just seems to make things worse.
“She became more agitated, wondering, well, ‘Where are you? Why aren’t you here? Come get me out of here,’ ” he says.
He begins to weep. “My calls were just creating more stress for her.”
Banning all nonessential people from nursing homes may have been a wise move at the beginning of the COVID-19 outbreak. But now the policy needs to be reconsidered, says Tony Chicotel, a staff attorney with California Advocates for Nursing Home Reform. For one thing, the ban hasn’t kept COVID-19 out of nursing homes.
“The virus finds its way into the building through whoever is coming in, whether it’s staff or visitors,” Chicotel says.
The coronavirus is likely to keep finding its way into nursing homes as long as it’s still in the community at large.
The Centers for Medicare & Medicaid Services have published guidelines for how nursing homes might reopen to visitors. Agency administrator Seema Verma confirmed in a conference call with reporters this month that it would be up to state and local leaders to set the rules.
Chicotel says his organization has a proposal he believes would work right now.
“For those family members who provide more than just companionship, who really provide support to that person’s quality of life in ways that the staff probably just can’t, those family members should have access to residents as long as they follow the same safety protocols that the staff are following,” Chicotel says. Those protocols would include wearing personal protective equipment and daily temperature checks.
Nancy Snider would have gladly done so. Her husband, Matt, was in a Michigan nursing home for years with Huntington’s disease.
“It’s one of the worst diseases someone can have,” she says. “And he’s battled it like a warrior for all these years.”
Either she, her daughter or a close family friend saw Matt every day. They performed a lot of tasks that most people would think were handled by the staff.
“We’d go in and if his shirt needed to be changed or his bedding wasn’t changed or if he still had some food from breakfast on his face, we would do that,” Nancy Snider says. “Just basically anything.”
Without that help and human contact, her husband’s decline was stunning. His weight dropped to about 90 pounds.
“The fact that no one called me about the change in his condition has really irritated me because it’s cost me time. It’s cost my family time with him,” Nancy Snider says. “It’s too late now. He’s actively dying.”
Shortly after we spoke, she moved him to a hospice facility that allowed family visitors. He died a few days later, with his wife and his daughter holding his hands.
Copyright 2020 NPR. To see more, visit NPR.
May 6, 2020. Hospitalizations Rise post Memorial Day
As the number of new coronavirus cases continues to increase worldwide, and more than a dozen states and Puerto Rico are recording their highest averages of new cases since the pandemic began, hospitalizations in at least nine states have been on the rise since Memorial Day.
In Texas, North and South Carolina, California, Oregon, Arkansas, Mississippi, Utah and Arizona, there are an increasing number of patients under supervised care since the holiday weekend because of coronavirus infections. The spikes generally began in the past couple weeks and in most states are trending higher.
Data from states that are reporting some of their highest seven-day averages of new cases is disproving the notion that the country is seeing such a spike in cases solely because of the continued increase in testing, according to data tracked by The Washington Post.
Many of these states that have experienced an increase in cases have also had an increase in hospitalizations, with a handful of states also nearing bed capacity. Hospitalizations nationwide are difficult to track, with states reporting hospitalization numbers in varying ways, or not at all. Even states that do report hospitalization numbers may not have always received complete data from every hospital in the state at the time of their reports.
Texas has reported 75,616 cases since the pandemic began, and in 10 of the past 15 days, the state’s seven-day average of new cases has increased.
As of Tuesday, it has reported two consecutive days of record-breaking coronavirus hospitalizations. The state has seen a 36 percent increase in new cases since Memorial Day, with a record 2,056 current hospitalizations as of early Tuesday afternoon. It was up from a high of 1,935 hospitalizations on Monday.
Texas was one of the first states to relax their stay-at-home order. Businesses started to open up in early May. According to the state’s health department, Texas has 28.14 percent of available hospital beds open, and 1,723 available intensive care unit beds.
In Arizona, 28,296 cases have been reported as of Tuesday, and in 13 of the past 15 days the state’s seven-day average of new cases has increased. There have been a record number of hospitalizations in the state over the past few days. As of Tuesday, Arizona reported 1,243 current hospitalizations, a 49 percent increase since Memorial Day, when there were 833 hospitalizations.
Arizona has also been struggling with its bed capacity. On Friday, Banner Health, one of the largest health-care systems in the country, confirmed that ICUs in Arizona were nearing capacity. Roughly 50 percent of all those hospitalized are in Banner Health facilities. As of Monday, 76 percent of all ICU beds in Arizona were in use, according to data from the state health department.
The most popular and interesting stories of the day to keep you in the know. In your inbox, every day.
Arkansas has reported 10,080 cases, and in 11 of the past 15 days the state’s seven-day average of new cases has increased. It has had an 88 percent increase in hospitalizations since Memorial Day. Arkansas had 173 hospitalizations reported on Tuesday, compared with 92 on May 25.
According to local reports, hospitals statewide remained below capacity on Monday, and none of the new coronavirus cases had been linked to recent protests in the state.
The Carolinas have also seen a rise in hospitalizations, with North Carolina experiencing the second-largest spike in the nation behind Texas. North Carolina’s upward trend began after Memorial Day. On May 26, the state reported 621 hospitalizations but two weeks later, that number has climbed to 774.
In South Carolina, hospitalizations sharply increased Monday. In that 24-hour span, there were 30 new hospitalizations, or a 6 percent jump, for a total of 507 covid-19 patients. With the current spike, 12 counties in South Carolina have reached 75 percent of hospital capacity or greater, according to the state’s health department.
Mississippi has reported 18,109 cases since the pandemic begin. On Tuesday, it recorded 671 hospitalizations, a new daily high. It has seen an 17 percent increase in hospitalizations since Memorial Day, with 573 reported on May 25.
In Utah, new covid-19 cases are on the rise and as a result, so are hospitalizations. Utah’s coronavirus task force tweeted that the state has seen a spike in coronavirus cases, and it wasn’t because of testing or a lone outbreak.
Similar to other regions, Utah’s numbers have climbed steadily since Memorial Day, as the seven-day average of new cases has increased 12 of the past 15 days. Over that two-week span, Utah’s current hospitalizations more than doubled, and as of Tuesday afternoon, 230 patients were hospitalized with covid-19.
Arizona tourist sites were packed for Memorial Day weekend. Lake Havasu, a popular vacation destination, was full, according to local officials. In South Carolina, a host of entertainment venues, including zoos, aquariums and water parks, were allowed to open the weekend ahead of Memorial Day. In North Carolina, restaurants were allowed to open at reduced capacity and public pools at 50 percent capacity during Memorial Day weekend.
As of Tuesday, at least 110,000 people in the United States have died of covid-19, the disease caused by the coronavirus, and almost 2 million cases have been reported.
May 6, 2020
May 6, 2020
7 things to know about COVID-19 antibody testing
BY Cynthia DeMarco
As more people recover from the novel coronavirus and seek to resume their normal activities, there’s been a lot of talk about testing for COVID-19 antibodies.
But what are antibody tests, exactly, and how do they differ from diagnostic tests for COVID-19? What do the results indicate for the people who take these tests? And what do they mean for how we should conduct ourselves during the COVID-19 pandemic?
To learn more about COVID-19 antibody testing, we spoke with Laboratory Director James Kelley, M.D., Ph.D. Here’s what he had to say.
What is antibody testing, and how does it differ from diagnostic testing used for COVID-19?
Diagnostic testing for COVID-19 involves looking to see whether an active virus is present — in this case, the coronavirus formally known as SARS-CoV-2. Laboratory technologists use a testing process to detect genetic material from the virus in samples swabbed from the very back of the nasal cavity. This testing is based on a common molecular testing technique: polymerase chain reaction (PCR).
By contrast, antibody testing (also called serology testing) is done with blood samples, because you’re looking for evidence of the body’s immune response to the virus.
After your body is exposed to a foreign pathogen, your white blood cells start to learn about it and make antibodies to neutralize it. So, when an antibody test comes back positive for this coronavirus, it means 1) you were exposed to SARS-CoV2 at some point in the past and 2) your immune system was robust enough to launch an antibody-forming immune response.
How long does it usually take people to generate these antibodies?
There are limited data related to antibodies against SARS-CoV2. Some reports suggest most healthy people start making antibodies 11 to 14 days after symptoms first appear.
But there are also other variables to consider, such as malnourishment, having cancer or another chronic health condition, or taking immune suppressing drugs. All of these can affect people’s ability to make antibodies.
What does a positive coronavirus antibody test result mean for someone in terms of immunity?
The short answer is we don’t know.
It may mean someone has full immunity or partial immunity or no immunity at all. Some antibodies decrease over time, so you might be immune for six months to a year, and then maybe not at all later on. Or, it might be like a tetanus immunization, where if you get it once, you’re most likely immune the rest of your life. There’s just no way to give definitive answers right now.
How long will it take before we know for sure what positive COVID-19 antibody test results really mean?
The answer to that question will take lots of research, and probably at least a year of data collection, to figure out. Because first, you need to find people with the COVID-19 antibody. Then, you need to follow them to see if they become infected again if they’re exposed to the virus in the future. And that takes time.
Why is it important for people not to assume they’re immune if they test positive for COVID-19 antibodies?
There’s a big difference between telling someone they have immunity versus that they may have immunity. That’s a really important distinction to make.
Because if someone says that they’re definitely going to give me a million dollars, I may go out and buy a new house. But if they tell me they may give me a million dollars, I probably won’t, because it’s not a promise. It’s only potential.
With this virus, we just don’t know the answer yet. We can only advise patients that they may have immunity if the antibody test is positive. So, even if I were to test positive for antibodies to the coronavirus, I wouldn’t change my behavior. I’d still wear personal protective equipment at work, wash my hands a lot and practice social distancing.
How accurate are the tests currently available?
The jury is still out on how good serology tests are for this coronavirus. They’re not used widely enough to have good answers yet.
A lot of companies are trying to market their tests right now. And some are making false claims to the point that the Food and Drug Administration may have to take action. It’s important to note that just because someone is saying they have a serology test, doesn’t necessarily mean you can trust that test to provide accurate results.
Here at MD Anderson, we’re looking at bringing in serology tests from some of the bigger, more established diagnostic equipment suppliers. We’re hoping to have those available in the coming weeks.
Where can people obtain antibody testing? And who should?
At MD Anderson, an antibody lab test requires orders from a physician. Antibody testing primarily reveals if you were exposed to SARS-CoV2 in the past and generated an antibody-forming immune response.
Until we know how antibody test results relate to immunity, the tests are mainly useful for epidemiologists and researchers. But as always, you should discuss your medical needs and any questions with your physician.
Learn more about COVID-19 and the precautions MD Anderson is taking.
May 4, 2020
April 21, 2020
Fort Bend County COVID 19 Update
April 20, 2020
AUSTIN, TX — Gov. Greg Abbott on Friday outlined a multi-pronged plan to gradually reopen the Texas economy currently stalled amid the new coronavirus outbreak — an initiative that includes keeping schools closed for the remainder of the academic year.
In mandating the extended schools closure, Abbott said online classes should continue to be utilized as an optional teaching method. The order directs all schools—including public, private, and higher education institutions — to remain closed for the 2019-2020 school year. Teachers may go into the classroom for video instruction, to perform administrative duties and to clean out their classrooms, the governor said.
Abbott also said state parks would be opened up again for public access as he cited their importance to mental health for those otherwise practicing self-isolation to help blunt the spread of illness. Despite the parks’ reopening scheduled for April 20, visitors must adhere to physical distancing guidelines, wear protective face coverings and limit groups to five or less, the governor explained.
Abbott’s plans to reignite the state economy by reopening businesses gradually comes amid growing illness counts and fatalities attributed to the respiratory illness. As of Thursday, the total number of patients afflicted with coronaivrus totals 16,445. Additionally, 29 more deaths were reported on Thursday from the previous 24-hour period.
The plan to reignite commerce in Texas — the world’s 12th largest economy — was sparked with three new executive orders to “to begin the process of reopening the state of Texas while revising hospital capacity and certain social distancing guidelines,” Abbott said.
To the end of restarting the economy, Abbott issued three new executive orders on Friday:
- The first order develops a strike force establishes the Strike Force to Open Texas — a team of nationally recognized medical experts and private and public leaders who will advise the governor on safely and strategically reopening the state of Texas.
- The governor’s second executive order relates to the “safe, strategic reopening” of select services and activities in Texas with establishment of a temporary “Retail-To-Go” model enabling retail outlets to reopen starting on Friday.
- The governor’s third executive order relates to hospital capacity and personal protective equipment (PPE) needed for the COVID-19 response.
‘Strike Force to Open Texas’ order
Effecting the plan will be the newly formed “Strike Force to Open Texas” comprising nationally recognized medical experts and private and public leaders advising the governor on safely and strategically reopening the state.
“Texans are battling a colossal challenge — an invisible enemy that has tested our lives and our livelihoods — but overcoming challenges is part of who we are as Texans,” Abbott said at a noon press conference outlining the plans. “We have shown that Texas can continue our efforts to contain COVID-19 while also adopting safe standards that will allow us to begin the process of reopening Texas. The Strike Force to Open Texas brings together nationally recognized medical experts with public and private sector leaders to achieve this mission. By coming together, we can get Texans back to work, practice safe standards that will prevent the spread of COVID-19, and we can overcome this pandemic.”
Leading the advisory “strike force” will be James Huffines while Mike Toomey will serve as chief operating officer. Lt. Gov. Dan Patrick, House Speaker Dennis Bonnen, Attorney General Ken Paxton and Comptroller Glenn Hegar will serve as consulting members, Abbott announced.
In addition, Abbott has appointed Texas Department of State Health Services Commissioner John Hellerstedt, MD, as Chief Medical Officer of the strike force. Dr. Hellerstedt will be supported by three Chief Medical Advisors:
- John Zerwas, MD, Executive Vice-Chancellor for Health Affairs at the University of Texas System.
- Mark McClellan, MD, PhD, Former Food and Drug Administration Commissioner and U.S. Medicaid and Medicare Administrator.
- Parker Hudson, MD, MPH, Assistant Professor of Internal Medicine and Infectious Diseases at Dell Medical School and program director for the Internal Medicine Residency.
Abbott said those health experts will develop a medical architecture to comprehensively test and trace COVID-19 that will enable Texans to gradually and safely begin the process of returning to work and other activities, he added.
The medical team will work alongside a special advisory council who will share innovative ideas to help businesses strategically reopen while containing the spread of the COVID-19 virus, the governor said. The council consists of 39 business leaders representing the state’s regions and industries. The advisory council will collaborate with working groups to devise strategies, statewide standards, and appropriate time frames to reopen the Lone Star State while prioritizing the health and safety of all Texans, the governor said.
The strike force will immediately begin providing input on potential additional openings of activities and services in Texas consistent with guidelines provided by the Centers for Disease Control and Prevention, Abbott explained. To that end, the governor said he would announce a revised plan for the state based on these initial recommendations on April 27.
Members of the governor’s Special Advisory Council include:
- Arcilia Acosta: President and CEO, CARCON Industries & Construction.
- Paul Andrews, Jr.: Founder and CEO, TTI Inc.
- Mark Bivins: Rancher, partner in Corsino Cattle Co.
- Kathy Britton: CEO and Owner, Perry Homes.
- Brad Brookshire: Chairman and CEO, Brookshire Grocery Co.
- J. Bruce Bugg, Jr.: Chairman, Texas Transportation Commission.
- Alonzo Cantu: President & CEO of Cantu Construction.
- Bobby Cox: Owner and operator, Bobby Cox Companies, Inc.
- Adriana Cruz: Executive Director, Economic Development & Tourism Division, Office of the Governor.
- Michael Dell: Chairman and CEO, Dell Technologies.
- Scott Dueser: Chairman, President & CEO, First Financial Bank.
- Don Evans: Chairman of the President George W. Bush Foundation, Chairman of Permian Strategic Partnership.
- Tilman Fertitta: Chairman, CEO, and sole owner, Landry’s, Inc.
- Richard Fisher: Senior Advisor, Barclays and Former President & CEO, the Federal Reserve Bank of Dallas.
- Rick Francis: Chairman of the Board, WestStar Bank Holding Company, Inc.
- Printice Gary: Founding Partner/Principal and CEO, Carleton Companies.
- Brad Heffington: Owner of Heffington Farms, Inc. and Triple T Irrigation, Inc.
- Jeffery D. Hildebrand: Executive Chairman and Founder, Hilcorp Energy Co.
- Nancy Kinder: President & CEO, Kinder Foundation.
- Tom Luce: Founder and Chairman, Texas 2036.
- Marc McDougal: CEO, McDougal Companies.
- Jim “Mattress Mack” McIngvale: Owner, Gallery Furniture.
- Drayton McLane: Chairman, McLane Group.
- Elaine Mendoza: Founder, President & CEO of Conceptual MindWorks, Inc.
- Balous Miller: Owner, Bill Miller Bar-B-Q Restaurants.
- Carla Moran: Ramar Communications.
- Dennis Nixon: CEO and Chairman of International Bank of Commerce.
- David Oliveira: Partner at Roerig, Oliveira & Fisher, L.L.P.
- Ross Perot, Jr.: Chairman, The Perot Group.
- Kevin D. Roberts, Ph.D.: Executive Director, Texas Public Policy Foundation.
- Robert B. Rowling: Owner and Chairman, TRT Holdings, Inc.
- Kendra Scott: Founder and CEO, Kendra Scott.
- Robert F. Smith: Founder, Chairman & CEO, Vista Equity Partners.
- Sam L. Susser: Chairman of BancAffiliated, Inc.
- Massey Villarreal: CEO and President, Precision Task Group, Inc.
- Kirk Watson: Founding Dean of the University of Houston Hobby School of Public Affairs.
- Marc Watts: President, The Friedkin Group.
- Graham Weston: Former Chairman of Rackspace Hosting Inc.
- Sanjiv Yajnik: President of the Financial Services Division, Capital One.
For more information about the Governor’s Strike Force to Open Texas, visit the strike force webpage.
‘Retail-To-Go’ model established for retailers
The governor’s second executive order related to the safe, strategic reopening of select services and activities in Texas establishes a temporary “Retail-To-Go” model enabling retail outlets to reopen starting on Friday, April 24. Under the model, reopened establishments are required to deliver items to customer’s cars, homes, or other locations to minimize contact.
3rd order loosens elective surgeries restrictions
The governor’s third executive order relates to hospital capacity and personal protective equipment (PPE) needed for the COVID-19 response. The order loosens restrictions on surgeries put in place by Gov. Abbott in March. To that end, beginning at 11:59 p.m. on April 21 through 11:59 p.m. on May 8, all licensed health care professionals and all licensed health care facilities must continue to postpone all surgeries and procedures that are not medically necessary to diagnose or correct a serious medical condition of, or to preserve the life of, a patient who without timely performance of the surgery or procedure would be at risk for serious adverse medical consequences or death as determined by a patient’s physician, Abbott said.
Exceptions now include:
- Any procedure that, if performed in accordance with the commonly accepted standard of clinical practice, would not deplete the hospital capacity or the PPE needed to cope with COVID-19, or
- any surgery or procedure performed in a licensed health care facility that has certified in writing to Texas HHSC both (1) that it will reserve at least 25% of its hospital capacity for treatment of COVID-19 patients, accounting for the range of clinical severity of COVID-19 patients, and (2) that it will not request any PPE from any public source—whether federal, state, or local—for the duration of the COVID-19 disaster.
Related stories:
Coronavirus: Austin, Travis County Urge Use Of Face CoveringsCoronavirus: Texas Illness Count Spikes To 16,455, 29 More DeathsCoronavirus: Austin Clarifies Rules After Governor’s OrdersCoronavirus: Shelter-In-Place Ordered For Austin AreaCoronavirus: Austin Bars, Restaurants Ordered To CloseCoronavirus: Texas Governor Orders Bars, Eateries, Schools Closed
In previously banning elective procedures to better accommodate coronavirus patients, Abbott included abortions as part of the restricted mix. Republican have long opposed the procedure, and pro-choice advocates were quick to criticize the inclusion of abortion in the list of restricted medical needs as one based solely on political ideology.
During Friday’s press conference, Abbott was asked whether the loosened rules apply to abortions, prompting a vague response: “We feel that we can begin allowing some procedures,” Abbott began. “In my conversation with the doctors before this decision was made, they were very cautious primarily because of the limited PPE
[personal protective equipment]still still for current hospital workers. Hence, it has opened up a little bit for more hospital procedures and for diagnotic tests — especially for those who may have serious illness in ways we do not think will compromise PPE supply in ways that will ensure there still will remain an adequate number of hospital beds for anybody who may test positive for COVID-19.”
After that response, the governor was pressed further if the now-loosened rules apply to abortions: “That is not part of this order,” Abbott acknowledged. “The way the order is written is in terms of what doctors write about the type of treatment that is provided.”
After the press conference, the Austin Chamber of Commerce issued a statement endorsing the governor’s plan. “As leaders of the Texas business community, we applaud Gov. Abbott for focusing on the incremental steps necessary to reopen the Texas economy,” Austin Chamber President and CEO Laura Huffman said in a prepared statement. “We recognize this effort will need to balance public health considerations while restarting economic activity in a phased and gradual approach that guards against subsequent spikes in infections.”
Huffman singled out the task force component as a critical cog of the plan to reignite the state economy: “While each of our communities is different, we recognize that businesses play a vital role in enacting specific measures to keep their workforce safe and thereby protecting the entire community,” the chamber president said. “We are encouraged by the governor’s willingness to work collaboratively with the business community. While COVID-19 will have long-term impacts on our state, smart policy decisions made now can greatly accelerate our economic recovery. We appreciate the governor’s leadership on this issue and look forward to working with the task force.”
Separately, Huffman noted:”We especially look forward to working with many of the Austin region’s own who have been appointed to the Governor’s Strike Force to Open Texas, including, former Austin Chamber board chair Sen. Kirk Watson, Michael Dell, Kendra Scott, Robert Smith and Adriana Cruz. We’re delighted former Austin Chamber board member James Huffines is leading this strike force. The work and insight these community and business leaders will provide is paramount to getting our region back to work.”
April 18, 2020
April 18, 2020
April 16, 2020
Stay 6 Feet Apart, We’re Told. But How Far Can Air Carry Coronavirus?
Most of the big droplets travel a mere six feet. The role of tiny aerosols is the “trillion-dollar question.”

By Knvul Sheikh, James Gorman and Kenneth Chang
The rule of thumb, or rather feet, has been to stand six feet apart in public. That’s supposed to be a safe distance if a person nearby is coughing or sneezing and is infected with the novel coronavirus, spreading droplets that may carry virus particles.
And scientists agree that six feet is a sensible and useful minimum distance, but, some say, farther away would be better.
Six feet has never been a magic number that guarantees complete protection. The Centers for Disease Control and Prevention, one of the organizations using that measure, bases its recommendation on the idea that most large droplets that people expel when they cough or sneeze will fall to the ground within six feet.
But some scientists, having looked at studies of air flow and being concerned about smaller particles called aerosols, suggest that people consider a number of factors, including their own vulnerability and whether they are outdoors or in an enclosed room, when deciding whether six feet is enough distance.
Sneezes, for instance, can launch droplets a lot farther than six feet according to a recent study.This 3-D Simulation Shows Why Social Distancing Is So ImportantWe visualized a cough to show how far respiratory droplets can spread. If you haven’t been keeping your distance to fight the coronavirus, this may persuade you.
No scientists are suggesting a wholesale change in behavior, or proposing that some other length for separation from another human, like seven, or nine feet, is actually the right one.
“Everything is about probability,” said Dr. Harvey Fineberg, who is the head of the Standing Committee on Emerging Infectious Diseases and 21st Century Health Threats at the National Academies of Sciences, Engineering and Medicine. “Three feet is better than nothing. Six feet is better than three feet. At that point, the larger drops have pretty much fallen down. Maybe if you’re out of spitting range, that could be even safer, but six feet is a pretty good number.”
One complicating factor is that aerosols, smaller droplets that can be emitted when people are breathing and talking, play some role in spreading the new coronavirus. Studies have shown that aerosols can be created during certain hospital or laboratory procedures like when using nebulizers to help patients inhale medication, which makes such procedures risky for doctors who do them.
If the aerosols that people exhale in other settings are significant in spreading the disease, the six-foot distance would not be completely protective because those are carried more easily by air currents.
Aerosols are generally considered to be particles under 5 microns in diameter, about the size of a red blood cell, and can be spread in the environment by talking and breathing. But some researchers argue that this is a false dichotomy. Infectious droplets can’t easily be divided into those that are big enough to fall to the ground quickly and those that stay aloft because so much depends on environmental conditions and how deeply they penetrate into the respiratory tract.Sign up to receive an email when we publish a new story about the coronavirus outbreak.
“It’s really a continuum,” said Dr. Donald Milton, who studies bioaerosols at the University of Maryland School of Public Health.
Even without the launching power of a sneeze, air currents could carry a flow of aerosol sized virus particles exhaled by an infected person 20 feet or more away.
“In any confined geometry like an office room, meeting room, department store, food store,” said Eugene Chudnovsky, a physicist at the City University of New York. In a study not yet peer reviewed, he analyzed air flow and showed how, “the vortices in the air are taking the virus to different places.”
A preliminary study at the University of Nebraska Medical Center found evidence of coronavirus genetic material on various surfaces in isolation rooms where infected patients were being treated, including on air vents more than six feet from the patients. The research, which has not yet been peer reviewed, indicates that the virus can occasionally travel long distances.
“The virus is so small, it can hitch a ride even on tiny, tiny particles,” Dr. Fineberg said. “But how important is each size and how well they can transmit disease is not fully understood.”
It is also unclear how many virus particles it takes to start an infection, how long the viral particles remain viable or if studies like the one in Nebraska simply detected the genetic calling card the virus left behind.
Spacing is an effective solution because it also reduces the number of people in a confined space. That reduces the likelihood of an infected person being in the group. And if there is one, fewer other people might be infected.
Dr. Michael Osterholm, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, said the six-foot distance would clearly “reduce the number of droplets you come in contact with. I have no doubt about that.”
But, he said: “The question is what does it take for you to get infected? And that I think is the trillion-dollar question we have.”
He said, “Maybe all it takes is an aerosol. You don’t need any droplets at all.” If that’s the case, he said, then someone who is at high risk would not want to be in the same room with someone who is infected or might be infected.
Current guidelines already suggest that anyone at high risk should stay home and not be out in public in the first place. And they seem to be working. Places where people reduced travel and started social distancing weeks ago, especially in California, New York and Washington, are starting to show a reduction in the number of new coronavirus cases.
People still need to shop and take care of necessities, Dr. Osterholm said, but reducing the risk of exposure to all possible modes of transmission — infected surfaces, droplets and smaller aerosols — is important.
“Your job is to limit it as much as you can.”
April 15, 2020
Hydroxychloroquine Discussion
April 15, 2020
Stimulus Checks and On Line Tracking System
With millions of Americans eagerly awaiting their federal stimulus checks to help them weather the the coronavirus recession, people are now able to find out when they can expect to get their money after the government on Wednesday launched a tracking tool called “Get My Payment.”
The first batch of stimulus checks — or “economic impact payments,” as they are officially known — started hitting consumers’ bank accounts on Saturday, the Internal Revenue Service has said. But millions of people remain unsure of when the payments will arrive because it depends on whether the IRS has your direct-deposit information and your income level. Consumers can also update their mailing addresses if they’ve moved since they last filed their tax returns.
The “Get My Payment” service went live on Wednesday at IRS.gov. It allows consumers to check their payment status, confirm whether they prefer direct deposit or a paper check and enter their bank account information for direct deposit if the IRS doesn’t have it yet.
“We expect over 80 million hard-working Americans will get the direct deposit by this Wednesday,” Mnuchin said.
Consumers will need either their 2019 or 2018 tax returns to complete the “Get My Payment” service, the IRS says. Taxpayers who haven’t yet filed for either year but are required to file a tax return will need to file their 2019 return to get their payment, the IRS said.
People who aren’t required to file tax returns, such as some on Social Security, can use this site for non-filers where they can send the IRS their direct deposit information.
How much you’ll get
Adults with income below $75,000 are due to receive $1,200 each, while married couples earning less than $150,000 will receive $2,400.
Roughly 9 in 10 American households will get a stimulus check, which is to help people stay afloat financially during the economic downturn caused by the pandemic. But certain factors could affect how much you get, as well as how fast you receive payment.
For one, single Americans who earn over $75,000 or married couples who earn above $150,000 will see their payments decline by $5 for every $100 over those amounts, until the payments phase out entirely at $99,000 and $198,000 for singles and couples, respectively.
Families with children under 17 years old will receive $500 per child — a calculation that leaves out many high school seniors. And adults who can be claimed as dependents, such as many college students, also won’t receive a stimulus check. Nonresident aliens, or those without a green card, are also excluded from the payments.
April 14, 2020
HOUSTON, Texas (KTRK) — Texas is seeing more people recovering from the coronavirus as more cities open up testing sites.
In newly released data from the state health department, 2,580 Texans have already recovered from COVID-19, as of Tuesday.
Lawmakers across the state have been pushing for testing as federal aid continues to come in.
Congresswoman Sheila Jackson Lee announced her push for testing, specifically at the Harris County Jail, while opening a free testing site on Houston’s south side where testing began on Monday.
In total, Texas is reporting up to 14,624 cases with 1,409 patients in hospitals across the state.
Although more than half of all counties in the state are reporting cases now, there are a handful that haven’t reported a case at all.
As of Tuesday, one of the counties that has not reported a case is Houston County, which is about halfway between the city of Houston and Dallas and covers a portion of the Davy Crockett National Forest.
Others include Madison, Sabine, Freestone and Refugio counties.
The city of Houston continues to lead the state in cases with 3,747 in total so far. Dallas is second with 1,788 cases while Fort Worth has moved into third place with 876 cases.
Austin is now fourth with 856 cases and San Antonio ranks fifth with 794 cases.
April 14, 2020
Coronavirus In Greater Houston: City Expands Testing To Anyone Who Wants It, Regardless Of Symptoms
As Houston enters its sixth week dealing with the coronavirus, Houston Public Media provides more live updates.Paul DeBenedetto / Matt Harab / Haya Panjwani, HPM Intern | Posted on April 13, 2020, 4:17 PM (Last Updated: April 13, 2020, 5:07 PM)
THE LATEST
- There are now more than 5,000coronavirus cases in the region, in Houston, greater Harris County, Fort Bend County, Montgomery County, Brazoria County, Liberty County, Chambers County, Galveston County, Austin County and Waller County.
- The city has opened drive-through testing sites to anyone, regardless of symptoms. You can call 832-393-4220 for a unique identification number, and directions to a testing site.
Updated 4:16 p.m. CT Monday
All city-run coronavirus testing sites in Houston will now be open to everyone, regardless of symptoms, as health officials try to get ahead of the spread of the COVID-19 pandemic, now entering its sixth week in the region.
The city is running two drive-through testing sites, both previously reserved for first responders and people with multiple symptoms of COVID-19.
But easing qualifications to receive a test is crucial, because asymptomatic carriers are just as likely to pass on the virus as symptomatic carriers, Dr. David Persse with the Houston Health Department.
“We’ve learned unfortunately that this virus is different in that aspect,” Persse said Monday, at the opening of a new testing site. “Sites like these who are taking asymptomatic, or without any symptoms, have given us incites that several weeks ago we did not anticipate.”
The new testing site opened at Cullen Middle School in Southeast Houston, an area that health officials consider a “hot spot” for the virus.
The process of receiving testing remains the same, and people looking to get tests were asked to call 832-393-4220 for a unique identification number, and directions to a testing site.
The Mayor’s Office for People with Disabilities is working on accommodating those with disabilities in getting to the sites.
Mayor Sylvester Turner also responded to suggestions from President Donald Trump and Gov. Greg Abbott to potentially lift orders limiting travel and business in Texas and other states, saying the city was listening to the advice of medical professionals, and working to further increase testing.
“I think we’re all anxious to get to the point where we can ‘reopen,’ whatever that means,” Turner said. “Whenever we get to that point to reopen, it won’t mean that everything just opens up at one time. And as you’ve heard people say, it’s not like you turn on the light, or the switch, and the lights just turn on. Whenever we get to that point, it will be very phased.”
The city on Monday announced 118 new COVID-19 cases and 2 more deaths, bringing the death toll in Houston to 18. All those who died had preexisting conditions, Turner said.
April 14, 2020
April 13, 2020
April 13, 2020
Gabrielle Elise Jimenez
Liquid Love
As a hospice nurse, part of the comfort I provide for both patients and their families, is a long lingering hug that says, “I got you, I am here for you, you are not alone”. Most times it is for them, but the truth is, I benefit from them as well, in fact sometimes, it is the only thing that helps me work through my own personal reaction after last breaths have been taken. But we can’t hug any more… and I struggle with this.
As this virus races through our world attempting to knock down everything in its path, it doesn’t take into consideration the already fragile population who are ill and dying. Doors to facilities are closed and on lock down leaving patients feeling alone and abandoned and loved ones feeling guilty and helpless. Families are afraid to let us into their homes, so many visits are refused, and time spent with our patients is limited. Families can’t gather to say goodbye, they don’t get the chance for last words, and many patients are dying alone, all of which goes against everything we strive for.
I decided this virus was not going to change who I am, and it was not going to get in my way when it comes to being there for someone at the end of their life. I refused to be another one of its victims, it was not going to stop me from providing the care I think all human beings deserve when they are dying. I would figure out a way to provide comfort and support, just differently.
So when I was called to see a patient who was agitated, restless, experiencing shortness of breath and actively dying, I donned double masks and gloves and provided the very best care I could. With medication, repositioning, comfort care and verbal reassurance that I would get him through this, his symptoms were relieved, and he was able to have a more peaceful dying process. His son-in-law, who had left his wife and kids back at home to come care for a man he considered a father, a brother and a friend was also struggling. The realization of him dying was finally hitting him and he started to cry. I reached out with my double gloved hands and I put mine on his and held it there… he too needed to know he was not alone.
Moments before the last breaths were taken, I had his son-in-law call his wife so that she could be with her father when he died. I was on one side of the bed, his son-in-law on the other, each of us holding a hand, six feet apart from each other, while his daughter said her last goodbyes over the phone. And while this was not our preferred way, his death was without distress, it was full of compassion and kindness and he was not alone. His son-in-law hung up the phone with his wife and started to cry. My instinct is always to offer a long, lingering hug but instead, I reached over, placed my hand on his and reminded him that to feel this ache… is to have known great love and I kept my hand there while he cried. In many ways, that was a long, lingering hug.
We sat, six feet apart, and talked about their relationship. I provided active listening, a safe place to remember and to feel, and the reminder that he was not alone, and his feelings were valid. Two of his neighbors came by to pay their respects, each wearing masks and gloves, each taking turns coming in the room, honoring protocols the best they could. One of his friends started to sob… and he said, “liquid love, that’s what these tears are, so much liquid love”. Their visits were brief, there were no hugs, no one touched, distance was respected, safety protocols were in place, and yet love still filled the room and he was honored and given a proper farewell.
I left there that night feeling comforted inside knowing that even with the barriers and protocols, I was still able to provide the kind of hospice care that fills my heart. I know we can’t do this for everyone, I know we need to honor and respect the rules right now. But this inspired me to try and find new ways to allow families to say goodbye, to allow patients to die in peace, and to find a creative way to ensure that no one dies alone… despite the current obstacles.
April 9, 2020
April 7, 2020
April 6, 2020
April 6, 2020
April 6, 2020
Coronavirus In Greater Houston: City Announces 10th Death, COVID-19 Reported In Assisted-Living Facility
As Houston enters its fifth week dealing with the coronavirus, Houston Public Media provides more live updates.Paul DeBenedetto | Posted on April 5, 2020, 6:31 PM

THE LATEST
- Houston announced its 10th death related to the coronavirus Sunday.
- Galveston announced its first death related to the virus Saturday.
- There are now at least 1,854coronavirus cases in the region, in Houston, greater Harris County, Fort Bend County, Montgomery County, Brazoria County, Liberty County, Chambers County, Galveston County and Waller County.
This story is part of Houston Public Media’s ongoing coronavirus coverage. To see our previous live coverage, click here. For more stories and information about the coronavirus, visit our Houston Ready project page.
Updated 6:28 p.m. CT Sunday
The city announced its 10th death related to the coronavirus over the weekend, while Galveston County announced its first, as the COVID-19 pandemic entered its fifth week in the Houston region.
The Houston Health Department announced Sunday that a man between 60 and 70 with underlying health condition was pronounced dead March 30, his death a result of the virus. Ten people in Houston have died of COVID-19, and the city now has 743 positive cases. Galveston County also announced a woman between 81 and 90 with underlying health conditions died Saturday.
There are more than 1,800 coronavirus cases in the greater Houston area, encompassing Harris, Galveston, Montgomery, Liberty, Brazoria, Waller, Fort Bend, Chambers and Austin counties.
Those cases include at least three new positive cases of COVID-19 in a southeast Harris County assisted living facility, including staff and residents, Harris County Public Health said Saturday. The county did not provide specifics on the facility or the people impacted.
The news came just one day after Galveston County announced a total of 83 people in a Texas City nursing home tested positive for COVID-19.
Although anyone can get the coronavirus, older adults, 65 years and older, are at higher risk for severe illness, according to the Centers for Disease Control and Prevention.
The region’s first coronavirus-related death, announced March 19, was in a northwest Harris County nursing home.
And in San Antonio, an outbreak at a San Antonio nursing home led to at least two deaths and 67 positive cases, according to Texas Public Radio.
As Houston enters its fifth week dealing with the coronavirus, Houston Public Media provides more live updates.Paul DeBenedetto | Posted on April 5, 2020, 6:31 PM

THE LATEST
- Houston announced its 10th death related to the coronavirus Sunday.
- Galveston announced its first death related to the virus Saturday.
- There are now at least 1,854coronavirus cases in the region, in Houston, greater Harris County, Fort Bend County, Montgomery County, Brazoria County, Liberty County, Chambers County, Galveston County and Waller County.
This story is part of Houston Public Media’s ongoing coronavirus coverage. To see our previous live coverage, click here. For more stories and information about the coronavirus, visit our Houston Ready project page.
Updated 6:28 p.m. CT Sunday
The city announced its 10th death related to the coronavirus over the weekend, while Galveston County announced its first, as the COVID-19 pandemic entered its fifth week in the Houston region.
The Houston Health Department announced Sunday that a man between 60 and 70 with underlying health condition was pronounced dead March 30, his death a result of the virus. Ten people in Houston have died of COVID-19, and the city now has 743 positive cases. Galveston County also announced a woman between 81 and 90 with underlying health conditions died Saturday.
There are more than 1,800 coronavirus cases in the greater Houston area, encompassing Harris, Galveston, Montgomery, Liberty, Brazoria, Waller, Fort Bend, Chambers and Austin counties.
Those cases include at least three new positive cases of COVID-19 in a southeast Harris County assisted living facility, including staff and residents, Harris County Public Health said Saturday. The county did not provide specifics on the facility or the people impacted.
The news came just one day after Galveston County announced a total of 83 people in a Texas City nursing home tested positive for COVID-19.
Although anyone can get the coronavirus, older adults, 65 years and older, are at higher risk for severe illness, according to the Centers for Disease Control and Prevention.
The region’s first coronavirus-related death, announced March 19, was in a northwest Harris County nursing home.
And in San Antonio, an outbreak at a San Antonio nursing home led to at least two deaths and 67 positive cases, according to Texas Public Radio.
April 4, 2020
83 Residents, Employees Test Positive For COVID-19 At Texas City Nursing Home
Health officials believe it may have been spread by employees who unknowingly had coronavirus.Katie Watkins | Posted on April 3, 2020, 6:31 PM (Last Updated: April 3, 2020, 6:53 PM)
Seventy additional residents and employees at a nursing home in Texas City have tested positive for COVID-19, bringing the total number of cases at the facility to 83, the Galveston County Health District announced Friday.
The first case of COVID-19 at The Resort at Texas City was reported on Saturday. After the cases climbed to 13 during the week, the health district and the University of Texas Medical Branch tested an additional 146 residents and employees on Thursday. Some of those results are still pending.
Galveston County Local Health Authority Dr. Philip Keiser said based on what they saw during a visit to the facility on Saturday, the staff is following CDC guidelines. He said they think the cases may have been spread by several employees.
“There’s no way that we can prove this, but we believe that there may have been some employees who had accidentally contracted COVID, and then had gone to work,” he said at a press conference Friday. “One of the things that we’re learning about this virus is that there are a lot more asymptomatic cases out there than anybody ever dreamed up. So it shouldn’t be surprising that this could happen at a place.”
The Resort at Texas City is a 135-bed facility about an hour southeast of Houston. Keiser said the nursing home has cohorted the patients together on a separate hallway away from everyone else.
He also said the health district is issuing an order requiring additional safety restrictions for long-term care facilities, including nursing homes and assisted living locations, in Galveston County during the pandemic.
“I think it’s important that given what we know now, and given what we know about the population of long-term care facilities and their vulnerability, that we double down so that we can protect them as best we can,” Keiser said.
Under the order, employees who work at a facility with a confirmed case will be prohibited from also working at other facilities.
“It was a surprise to us to realize, but this is a fairly common practice, people will often work at more than one facility,” Keiser said.
This has raised concerns that healthcare workers could be unknowingly spreading coronavirus across locations.
Keiser said there are a few other long-term care facilities in the county with a smaller number of confirmed cases.
The order also requires long-term facilities with positive cases to notify family members and “at the very least, put a sign on the front door letting the public know there is a COVID-19 positive resident within the facility,” the health district wrote in a release.
Long-term facilities will also be prohibited from taking residents outside the grounds except for in an emergency or for dialysis.
“We are gravely concerned about the spread of this virus within nursing homes because of the close proximity and vulnerability of the residents,” Keiser said in a press release announcing the first 13 cases Thursday.
In Montgomery County, The Conservatory at Alden Bridge, an apartment complex for seniors in the Woodlands, is also dealing with a coronavirus outbreak that has resulted in the death of three men.
April 3, 2020
April 1, 2020
US Naval Hospital sailing into NYC

April 1, 2020
Field Hospital in Central Park, NY

April 1, 2020
A service dog in training brings comfort to ER doctors on the frontlines
April 1, 2020
HOUSTON, Texas (KTRK) — A major Houston hospital is spearheading a crucial treatment in the ongoing battle against COVID-19. Houston Methodist is the first academic medical center in the nation to be approved by the FDA to transfuse donated plasma from a recovered COVID-19 patient into a critically ill patient.
The experimental treatment was fast-tracked as the death toll in the coronavirus pandemic soared to more than 2,000 people across the United States and more than 100,000 Americans sick from the virus, according to a statement.
The concept of the treatment centers around the idea that plasma from someone who has recovered from COVID-19 contains antibodies made by the immune system and is used to kill the virus. Transfusing antibody-rich plasma into a COVID-19 patient who is still fighting the virus may transfer the power of the antibodies into a healing, possibly life-saving therapy, according to the hospital.
April 1, 2020 How to Care for a Loved One with COVID-19
March 31, 2020
What do Older Adults and People with Disabilities Need to Know?
People who are 65 or older are more likely to have serious COVID-19 illness. This may be because immune systems change with age, making it harder to fight off diseases and infection. Older adults also are more likely to have underlying health conditions that make it harder to cope with and recover from illness.
In addition, people of any age who live in a nursing home or long-term care facility are at higher risk.
Other people who may be at higher risk for getting very sick from COVID-19, regardless of age or disability, include:
- People with chronic lung disease or moderate-to-severe asthma
- People who have serious heart conditions
- People with severe obesity (body mass index [BMI] >40)
- People with underlying medical conditions, particularly if not well controlled, such as those with diabetes, renal failure, or liver disease might also be at risk
- People who are immunocompromised. Many conditions can cause a person to be immunocompromised, including cancer treatment, smoking, bone marrow or organ transplantation, immune deficiencies, poorly controlled HIV or AIDS, and prolonged use of corticosteroids and other immune weakening medications including people receiving cancer treatment
Reducing exposure is especially important for people at higher risk of complications!Take actions to reduce your risk of getting sick
Words to the wise: Planning is key!
Many states and communities are implementing community actions designed to reduce exposures to COVID-19 and slow the spread of the disease. Creating a household plan can help protect your health and the health of those you care about. You should base the details of your household plan on the needs and daily routine of your household members. CDC’s planning resources can help.
Everyday actions to prevent illness
You can learn more about how the virus spreads here. Everyone, regardless of age or disability, should follow CDC’s recommendations to help prevent the spread of all respiratory diseases, including colds and flu and COVID-19. Things you can do every dayPresident’s Coronavirus Guidelines for America: 15 Days to Slow the Spread
Watch for symptoms and emergency warning signs
- COVID-19 symptoms include fever, cough, and shortness of breath. If you feel like you are developing symptoms, call your doctor.
- If you develop emergency warning signs for COVID-19 get medical attention immediately. These include:
- Difficulty breathing or shortness of breath
- Persistent pain or pressure in the chest
- New confusion or inability to arouse
- Bluish lips or face
- This list is not all inclusive. Consult your medical provider for any other symptom that is severe or concerning.
March 31, 2020
THANK YOU TO OUR HEROES
March 29, 2020
How to Keep Coronavirus out of your Home
March 29, 2020
Dr Fauci COVID 2019 Projections
Washington (CNN)The nation’s top infectious disease expert said Sunday that based on models, the United States could eventually see 100,000 or more deaths from the novel coronavirus, which has already claimed more than 2,000 American lives as cases surge across the US.”Whenever the models come in, they give a worst-case scenario and a best-case scenario. Generally, the reality is somewhere in the middle. I’ve never seen a model of the diseases that I’ve dealt with where the worst case actually came out. They always overshoot,” Dr. Anthony Fauci, a key member of the White House’s coronavirus task force, told CNN’s Jake Tapper on “State of the Union.” “I mean, looking at what we’re seeing now, you know, I would say between 100 and 200,000 (deaths). But I don’t want to be held to that,” he said, adding that the US is going to have “millions of cases.” The comments come as the number of reported coronavirus deaths doubled to more than 2,000 nationwide in two days. The US has the most confirmed cases worldwide, with more than 121,000 as of Saturday morning.During a Sunday evening news conference, President Donald Trump said that, based on models that the coronavirus outbreak could bring 100,000-200,000 deaths in the US, his administration would “have done a good job.”Trump also said Sunday he would extend nationwide social distancing guidelines for another 30 days. Fauci and White House coronavirus response coordinator Dr. Deborah Birx had long supported extending the guidelines and gave a strong presentation with the new models that showed the 100,000 to 200,000 people could die, a source familiar with the President’s decision told CNN.Still, there is concern among some skeptics in the White House that these models Birx put so much stock in could be wrong, just as others have been since so much is unknown, the source said. But the president wasn’t given much of a choice but to agree to more time, a source familiar with the President’s decision told CNN.A separate source familiar with the President’s decision said aides thought it was good to announce it on a Sunday night before a new week begins.INTERACTIVE: Tracking Covid-19 cases in the USFauci says Trump agreed not to invoke a strict quarantine after intensive White House discussionsFauci and other experts have said the crisis will get worse before it improves, and the recent uptick in cases has caused severe supply shortages for hospitals around the country, especially in New York, the state with the highest number of cases nationwide. Numerous hospitals across the country expect to run out of beds within two weeks as cases continue to rise. New York City Mayor Bill de Blasio told CNN Sunday that his city has enough supplies to only last a week.”We have enough supplies to get to a week from today with the exception of ventilators. We’re going to need at least several hundred more ventilators very quickly. But we have otherwise the supplies to get to next Sunday,” de Blasio told Tapper on the same program. “We are going to need a re-enforcement by Sunday, April 5 in all categories, especially ventilators but in other areas as well. And personnel is becoming more and more the issue.”In an effort to curb the spread of the virus, various cities and states — including New York — have implemented stay-at-home orders for their residents, which have now impacted at least 215 million Americans. On Saturday, the Centers for Disease Control and Prevention issued a travel advisory to New York, New Jersey and Connecticut, urging residents of the three states — which have a significant amount of the cases in the country — to “refrain from nonessential domestic travel for 14 days effective immediately.” This story has been updated to include Trump’s statement and additional developments Sunday.CLARIFICATION: The headline and this story have been updated to better convey that Dr. Anthony Fauci was offering a possible estimate based on his interpretation of the coronavirus models.
CNN’s Chandelis Duster contributed to this story.
March 29, 2020
Ebola, other past virus outbreaks help Katy-area hospitals prepare for coronavirus

Katy-area hospitals planned ahead for the coronavirus and are changing procedures to prepare for surge in cases. (Courtesy Adobe Stock)
By Jen Para | 2:31 PM Mar. 26, 2020 CDT | Updated 2:31 PM Mar. 26, 2020 CDT
Officials from Houston Methodist West Hospital, Memorial Hermann Health System and Texas Children’s Hospital West Campus said they first began preparing for the coronavirus months before it hit the U.S.
Texas Children’s Hospital confirmed as of March 25 it has adequate supplies and protective equipment, said Jaclyn Houghton, a Texas Children’s Hospital public relations specialist, in an email interview.
As of March 24, Houston Methodist West also has enough supplies and staff ready for the current case count—and a future surge—said Sarah Lam, Houston Methodist West Hospital’s senior marketing and communications specialist, in an email interview.
“The Ebola scare a few years ago was a useful trial run for us to handle these types of infectious disease events,” Lam said. “And our caregivers continually train, so we are prepared to handle the situation if we see an influx of patients.”
Memorial Hermann Health System—which has a Katy hospital—also cited previous outbreaks as situations that have helped it be ready for the coronavirus, said Drew Munhausen, a senior external communications specialist for Memorial Hermann-Texas Medical Center, in an email interview. RELATED STORIES
“Historical outbreaks of other infectious diseases, such as swine flu, Ebola and Zika, have strengthened Memorial Hermann’s ability to respond to infectious disease situations in terms of readiness and preparedness,” Munhausen said.
Additionally, Texas Children’s Hospital West Campus has a special isolation unit at its campus, Houghton said. This eight-bed unit, which offers biocontainment, is among the few in the U.S. specialized for pediatric patients under the age of 21, she added.
“This is designed specifically for patients with highly contagious infectious diseases, such as Ebola, MERS [Middle East respiratory syndrome, another coronavirus disease] and other special pathogens,” Houghton said. “This unit features a highly-trained team that is ready to care for any patient.”
The highly infectious disease unit at Houston Methodist Continuing Care Hospital in Katy also opened March 23, Lam said.
“This unit with 20 beds, and 22 more coming in the near future, will house the sickest COVID-19 patients,” Lam said. “We have an emergency response team at this location should we need them.”
Changing hospital processes
All three hospital systems have changed several procedures to offer additional capacity if the case count begins to rise quickly.
“While our biocontainment unit is eight beds, we are prepared to expand the specialized care we offer to admit additional COVID-19 patients as needed, safely,” Houghton said. “We do also have surge plans in place and will be here to care for the needs of children and high-risk women.”
She added Texas Children’s has 969 licensed beds as of March 25, though the number of available beds changes daily. All Texas Children’s campuses—following Texas Health and Human Services Commission guidelines—implemented limited visitation guidelines. Campuses have also reduced the number people on shuttles and enhanced daily sanitation and cleaning processes.
On March 23, Houston Methodist hospitals no longer conducted elective nonurgent surgeries and procedures, Lam said. Two days later, the hospitals stopped elective, nonurgent diagnostic and ancillary testing.
“Not performing the nonurgent surgeries and procedures will free up beds in case we need them in case of a surge,” Lam said.
Memorial Hermann Health System also postponed elective, nonurgent surgeries and procedures as directed for the U.S. surgeon general, Munhausen said.
“Postponing these surgeries and procedures conserves resources for the sickest and most vulnerable patients,” Munhausen said.
He added Memorial Hermann has isolation policies and rooms across its hospitals to safeguard others from exposure.
All three hospitals are also still helping patients who do not have the coronavirus.
Memorial Hermann is urging patients to use Memorial Hermann eVisits, which offers telemedicine 24/7 to help diagnose and treat minor illnesses, Munhausen said. Houston Methodist also offers telemedicine for nonemergency urgent care needs, and it is also treating individuals who arrive at its location, Lam said.
“We are taking care of all patients who come through our doors,” Lam said. “This is something we have always done and it’s something that will never change.” Tags: Houston Methodist West Hospital , Memorial Hermann Health System said , Katy , Katy Health Care , Coronavirus (COVID-19) , Drew Munhausen , Sarah Lam , Texas Children’s Hospital West , Jaclyn Houghton SHARE THIS STORY
March 27, 2020
What The World Needs Now
March 26, 2020 Say THANK YOU
March 26, 2020
Colorado Symphony Plays Virtual Concert
March 26, 2020
That Discomfort You’re Feeling Is Grief

We’ve made our coronavirus coverage free for all readers. To get all of HBR’s content delivered to your inbox, sign up for the Daily Alert newsletter.
Some of the HBR edit staff met virtually the other day — a screen full of faces in a scene becoming more common everywhere. We talked about the content we’re commissioning in this harrowing time of a pandemic and how we can help people. But we also talked about how we were feeling. One colleague mentioned that what she felt was grief. Heads nodded in all the panes.
If we can name it, perhaps we can manage it. We turned to David Kessler for ideas on how to do that. Kessler is the world’s foremost expert on grief. He co-wrote with Elisabeth Kübler-Ross On Grief and Grieving: Finding the Meaning of Grief through the Five Stages of Loss. His new book adds another stage to the process, Finding Meaning: The Sixth Stage of Grief. Kessler also has worked for a decade in a three-hospital system in Los Angeles. He served on their biohazards team. His volunteer work includes being an LAPD Specialist Reserve for traumatic events as well as having served on the Red Cross’s disaster services team. He is the founder of www.grief.com, which has over 5 million visits yearly from 167 countries.
Kessler shared his thoughts on why it’s important to acknowledge the grief you may be feeling, how to manage it, and how he believes we will find meaning in it. The conversation is lightly edited for clarity.
HBR: People are feeling any number of things right now. Is it right to call some of what they’re feeling grief?
Kessler: Yes, and we’re feeling a number of different griefs. We feel the world has changed, and it has. We know this is temporary, but it doesn’t feel that way, and we realize things will be different. Just as going to the airport is forever different from how it was before 9/11, things will change and this is the point at which they changed. The loss of normalcy; the fear of economic toll; the loss of connection. This is hitting us and we’re grieving. Collectively. We are not used to this kind of collective grief in the air.
You said we’re feeling more than one kind of grief?
Yes, we’re also feeling anticipatory grief. Anticipatory grief is that feeling we get about what the future holds when we’re uncertain. Usually it centers on death. We feel it when someone gets a dire diagnosis or when we have the normal thought that we’ll lose a parent someday. Anticipatory grief is also more broadly imagined futures. There is a storm coming. There’s something bad out there. With a virus, this kind of grief is so confusing for people. Our primitive mind knows something bad is happening, but you can’t see it. This breaks our sense of safety. We’re feeling that loss of safety. I don’t think we’ve collectively lost our sense of general safety like this. Individually or as smaller groups, people have felt this. But all together, this is new. We are grieving on a micro and a macro level.
What can individuals do to manage all this grief?
Understanding the stages of grief is a start. But whenever I talk about the stages of grief, I have to remind people that the stages aren’t linear and may not happen in this order. It’s not a map but it provides some scaffolding for this unknown world. There’s denial, which we say a lot of early on: This virus won’t affect us. There’s anger: You’re making me stay home and taking away my activities. There’s bargaining: Okay, if I social distance for two weeks everything will be better, right? There’s sadness: I don’t know when this will end. And finally there’s acceptance. This is happening; I have to figure out how to proceed.
Acceptance, as you might imagine, is where the power lies. We find control in acceptance. I can wash my hands. I can keep a safe distance. I can learn how to work virtually.
When we’re feeling grief there’s that physical pain. And the racing mind. Are there techniques to deal with that to make it less intense?
Let’s go back to anticipatory grief. Unhealthy anticipatory grief is really anxiety, and that’s the feeling you’re talking about. Our mind begins to show us images. My parents getting sick. We see the worst scenarios. That’s our minds being protective. Our goal is not to ignore those images or to try to make them go away — your mind won’t let you do that and it can be painful to try and force it. The goal is to find balance in the things you’re thinking. If you feel the worst image taking shape, make yourself think of the best image. We all get a little sick and the world continues. Not everyone I love dies. Maybe no one does because we’re all taking the right steps. Neither scenario should be ignored but neither should dominate either.
Anticipatory grief is the mind going to the future and imagining the worst. To calm yourself, you want to come into the present. This will be familiar advice to anyone who has meditated or practiced mindfulness but people are always surprised at how prosaic this can be. You can name five things in the room. There’s a computer, a chair, a picture of the dog, an old rug, and a coffee mug. It’s that simple. Breathe. Realize that in the present moment, nothing you’ve anticipated has happened. In this moment, you’re okay. You have food. You are not sick. Use your senses and think about what they feel. The desk is hard. The blanket is soft. I can feel the breath coming into my nose. This really will work to dampen some of that pain.
You can also think about how to let go of what you can’t control. What your neighbor is doing is out of your control. What is in your control is staying six feet away from them and washing your hands. Focus on that.
Finally, it’s a good time to stock up on compassion. Everyone will have different levels of fear and grief and it manifests in different ways. A coworker got very snippy with me the other day and I thought, That’s not like this person; that’s how they’re dealing with this. I’m seeing their fear and anxiety. So be patient. Think about who someone usually is and not who they seem to be in this moment.
One particularly troubling aspect of this pandemic is the open-endedness of it.
This is a temporary state. It helps to say it. I worked for 10 years in the hospital system. I’ve been trained for situations like this. I’ve also studied the 1918 flu pandemic. The precautions we’re taking are the right ones. History tells us that. This is survivable. We will survive. This is a time to overprotect but not overreact.
And, I believe we will find meaning in it. I’ve been honored that Elisabeth Kübler-Ross’s family has given me permission to add a sixth stage to grief: Meaning. I had talked to Elisabeth quite a bit about what came after acceptance. I did not want to stop at acceptance when I experienced some personal grief. I wanted meaning in those darkest hours. And I do believe we find light in those times. Even now people are realizing they can connect through technology. They are not as remote as they thought. They are realizing they can use their phones for long conversations. They’re appreciating walks. I believe we will continue to find meaning now and when this is over.
What do you say to someone who’s read all this and is still feeling overwhelmed with grief?
Keep trying. There is something powerful about naming this as grief. It helps us feel what’s inside of us. So many have told me in the past week, “I’m telling my coworkers I’m having a hard time,” or “I cried last night.” When you name it, you feel it and it moves through you. Emotions need motion. It’s important we acknowledge what we go through. One unfortunate byproduct of the self-help movement is we’re the first generation to have feelings about our feelings. We tell ourselves things like, I feel sad, but I shouldn’t feel that; other people have it worse. We can — we should — stop at the first feeling. I feel sad. Let me go for five minutes to feel sad. Your work is to feel your sadness and fear and anger whether or not someone else is feeling something. Fighting it doesn’t help because your body is producing the feeling. If we allow the feelings to happen, they’ll happen in an orderly way, and it empowers us. Then we’re not victims.
In an orderly way?
Yes. Sometimes we try not to feel what we’re feeling because we have this image of a “gang of feelings.” If I feel sad and let that in, it’ll never go away. The gang of bad feelings will overrun me. The truth is a feeling that moves through us. We feel it and it goes and then we go to the next feeling. There’s no gang out to get us. It’s absurd to think we shouldn’t feel grief right now. Let yourself feel the grief and keep going.

Scott Berinato is a senior editor at Harvard Business Review and the author of Good Charts Workbook: Tips Tools, and Exercises for Making Better Data Visualizations and Good Charts: The HBR Guide
COVID-19 Food Safety Tips
March 24, 2020 Tracking COVID 19 Map
By Tuesday, the novel coronavirus outbreak in the United States had grown to at least 53,740 cases in all 50 states, the District of Columbia and Puerto Rico. There are outbreak clusters in New York, Washington State and California, according to Johns Hopkins University, which is tracking reports and confirming them with local health departments.
The number of cases in the U.S. and worldwide is the subject of some debate, as testing has been rolled out unevenly and the criteria for diagnosis (through clinical means or a lab test) has varied from country-to-country.
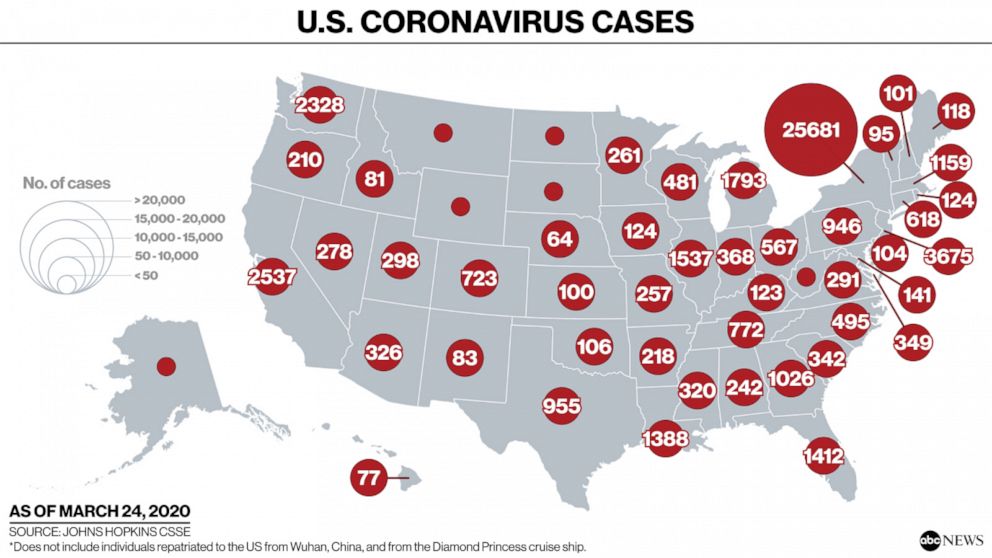
For more information on COVID-19 cases in your state, check your state’s health department website, listed below. The U.S. Centers for Disease Control and Prevention maintains nationwide statistics, but they are not updated as frequently. Information from Johns Hopkins University is not independently verified by ABC News.
The growing number of lab-confirmed cases in the U.S. at this point still pales in comparison to the seasonal flu, which kills an estimated 12,000 to 61,000 people per year and affects between 9 million and 45 million people in the country, according to the CDC.
Still, experts warn that the COVID-19 shouldn’t be downplayed or compared to a bad case of the flu. Instead, the respiratory disease is more akin to severe pneumonia, and in serious cases, patients experiencing difficulty breathing have been hospitalized and put on ventilators.
March 24, 2020 Doctors and Music
COVID-19 Basic Video
Hospices Struggle to Access Patients in Nursing Homes Amid Pandemic
By Holly Vossel | March 20, 2020
CDC
With older adults suffering from chronic or life-limiting medical conditions among those most vulnerable during the COVID-19 outbreak, nursing homes across the country are restricting access to their facilities. As a result, hospice providers have experienced difficulty accessing their patients in nursing home settings.
Nursing home populations are at the highest risk of being affected by the coronavirus, according to the U.S. Centers for Disease Control and Prevention (CDC). To address pandemic spread concerns, the U.S. Center for Medicare & Medicaid Services (CMS) announced critical measures last week to keep nursing home residents safe from exposure to COVID-19.
“About 10% of our 70 nursing homes here in Pinellas County [Florida] are not allowing hospice personnel access to our hospice patients residing in nursing homes,” said Scott Kistler, vice president of strategy and business development for Empath Health, a Florida-based hospice and palliative care service provider. “And that’s not particular to us. It’s a widespread problem.”
The new CMS recommendations advised nursing homes to “significantly restrict visitors and nonessential personnel, as well as restrict communal activities inside nursing homes” to protect seniors at the highest risk for complications from COVID-19.
As nursing homes work to protect both patients and staff in accordance with the CMS and CDC guidelines, volunteers, visitors, therapists, and various other contractors are included in the restrictions. While CMS Administrator Seema Verma indicated that hospice workers among those considered essential personnel who should be allowed access, it’s unclear how many nursing homes are aware of this specification.
Though the access problems are widespread, they are not universal. Some nursing homes are continuing to let in hospice clinicians.
“Facilities can establish their own guidelines on restricted visitation,” said Jeri Krauss, an independent geriatric nurse consultant in Texas specializing in hospice care . “Most that I have talked to are allowing family and care workers to see residents on hospice care. Workers and family wear personal protective equipment (PPE) during the visit.”
To continue providing patients with end-of-life care during the COVID-19 pandemic, hospices are working with nursing homes to gain access and reassure them of protective measures being taken against the risks.
“Our partners in nursing homes and assisted living facilities are continually working to ensure the safety of their patients and staff,” VITAS Healthcare indicated to Hospice News in an email. “As part of this advocacy, we ensure our clinicians follow adequate hand hygiene and adhere to facility screening procedures, as well as working with facility leadership to incorporate CDC and CMS guidance. Educational material was also developed to instruct on proper cleaning and disinfection procedures.”
VITAS Healthcare is a subsidiary of Chemed Corp., (NYSE: CHE).
With a shared focus on quality care for vulnerable patients, some nursing homes and long term care providers are working to expand their definition of essential personnel to include hospice providers.
“Hospice providers are a key part of the senior care health team, and we work in collaboration to enhance quality of life in the final months of life,” said Erin Shvetzoff Hennessey, CEO of Health Dimensions Group, a consulting and management service provider to long-term care and senior living operators in Minnesota. “We need hospice providers to continue to provide the holistic support to our residents and their families as they always do.”
Ramping up protective measures has been among the most vital actions hospices are taking to reassure safety and reduced risk when entering nursing home facilities.
“Most of our nursing homes here are screening and temperature-screening staff that are coming in,” said Laura Mosby, vice president of compliance and organizational excellence with Empath Health. “All staff going into nursing homes and assisted living support are going to be required to wear procedural masks and gloves if they’re providing direct care to a patient. The flip side to that is that we will blow through our supply. It’s now created a different concern: Will we be able to sustain enough medical supplies to meet this requirement?”
With this concern in mind, the CDC issued new guidance on the use of masks, gowns and face shields including suggestions on what to do if in crises shortages when supplies are exhausted. Nursing homes and assisted living communities are encouraged to significantly conserve masks and gowns in order to extend availability of remaining PPE supply.
Additional measures involve providing nursing home patients with reassurance to continue receiving the care they need.
“We are communicating with our residents to remind them that their needs will continue to be met and that essential health care services, including hospice services, will be continued without interruption,” said Shvetzoff Hennessey. “They are also reassured that all visitors to the community, even those for end-of-life visits or essential care workers, are being screened for illness in an effort to reduce their exposure to COVID-19.”
Equally as important to accessibility is the well-being and health of hospice staff accessing nursing homes. As staff entering facilities and patient homes take precautionary action to protect patients, their own health is just as vital to safeguard colleagues and their families.
With unprecedented school closings during the COVID-19 outbreak, hospice staffing support is extending beyond physical health protection and into personal life needs as well. Many families who rely on school-provided meals are experiencing food shortage issues. Additionally, staff are experiencing financial strain with unemployment numbers on the rise as businesses nationwide shut down during the pandemic.
“You have to take care of your staff and help them feel confident and competent, they then have the resources they need to be able to take care of patients and their families,” said Mosby. “One of the things that we’re working on right now is putting together some resource materials for our staff to give them access to whatever they need to be able to continue to work and live with the least amount of disruption as possible.”
As the coronavirus pandemic surges, hospices and nursing homes need to continue a collaborative partnership and provide patients with accessible care.
“At times like this, it requires those of us who are in leadership roles to really address those fears and anxiety within our staff and our volunteers so that they can in turn calm the fears and anxieties of our patients and families,” Kistler told Hospice News. “The population that we care for, many of these people would not be able to survive this virus, and also to the patients who may contract the virus and to their families who would be challenged by that. It really is a call to action to continue providing the best care possible in these vulnerable populations.”
Doffing Personal Protective Equipment (PPE) – Gown
See a demonstration of how to safely remove a gown in order to prevent infection.
https://www.jointcommission.org/covid-19/doffing-personal-protective-equipment-ppe—gown/
The number of Houston-area coronavirus cases stands at 199 with 2 deaths, 19 recoveries reported
:strip_exif(true):strip_icc(true):no_upscale(true):quality(65)/arc-anglerfish-arc2-prod-gmg.s3.amazonaws.com/public/CPEGHRMGCZHPLAXM22OYVMOAYQ.png)
HOUSTON – Here is a quick look at the coronavirus cases that have been reported in the Greater Houston area.
Here is a breakdown of the total number of coronavirus cases that have been reported in the Houston area. Deaths and recoveries are included in the total number of cases for each location.
| County or City | Total Cases | Deaths | Recoveries |
|---|---|---|---|
| Brazoria County | 18 | ||
| Brazos County | 12 | ||
| Chambers County | 1 | ||
| Fort Bend County | 42 | 4 | |
| Galveston County | 18 | ||
| Grimes County | 2 | ||
| Harris County | 54 | 1 | 12 |
| Houston (city) | 24 | 2 | |
| Liberty County | 1 | ||
| Matagorda County | 6 | 1 | 1 |
| Montgomery County | 19 | ||
| Walker County | 1 | ||
| Waller County | 0 | ||
| Wharton County | 1 | ||
| HOUSTON-AREA TOTAL | 199 | 2 | 19 |
Brazoria County: 18 total cases
The total number of reported coronavirus cases is at 18.
Here is the information provided by Brazoria County health officials about the cases:
- A male between the ages of 30-40 and resides in Angleton. He is in stable condition.
- A male between the ages of 60-70 and resides in Rosharon. He is in stable condition and recovering in home isolation. Not travel related.
- A female, between the ages of 20-30 and resides in Angleton, is in stable condition and recovering in home isolation.
- A male, between the ages of 50-60 and he resides in Pearland, is in stable condition and recovering in home isolation.
- A man, between the ages of 25-35 that resides in Angleton, is in stable condition and recovering in home isolation.
- A man, between the ages of 55-65 that resides in Clute, is in stable condition and recovering in home isolation.
- A man, between the ages of 20-30 that resides in Rosharon, is in stable condition and recovering in home isolation.
- A man, between the ages of 50-60. He resides in Pearland and is at home recovering in isolation. This case is not travel related.
- A man, between the ages of 45-55 who lives in Pearland. He is isolated at home. Has a history of travel
- A man, between the ages of 40-50 who lives in Pearland and is now in self-isolation. Has a history of travel
- A man between the ages of 40-50 who lives in Pearland and is at home recovering in isolation. Has a history of travel
- A woman, between the ages of 65-75 who lives in Pearland and is at home recovering in isolation. Has a history of travel
- A man between the ages of 50-60 who lives in Alvin and is at home recovering in isolation. Has a history of travel
- A man between the ages of 40-50, and resides in the Rosharon area. The individual is not hospitalized and is recovering at a private residence.
- A man between 55 and 65 years old who lives in the Manvel area. He is hospitalized and in stable condition.
- A woman between 50 and 60 years old who lives in the Pearland area. Her illness is believed to be related to travel.
- Two people who live in the Alvin area who attended the Houston Rodeo cookoff.
Brazos County: 12 total cases
The number of coronavirus cases that have been reported in Brazos County is at 12.
Here is the information Brazos County health officials have released thus far about the cases:
- 4 cases were announced Saturday, March 21. Details on the new cases were not provided.
- A man in his 30s with no travel history
- A man in his 20s who traveled to Mexico
- A woman in her 20’s who traveled to Spain. She is isolated at home.
- A man in his 60’s who traveled to Colorado. He is isolated at home.
- A woman in her 20’s who traveled to New York. She is isolated at home.
- A woman in her 50’s who traveled to Colorado. She is isolated at home.
Chambers County: 1 total case
The Chambers County Public Health confirms its first positive coronavirus case.
- The female patient is between 50-60 years old and lives in West Chambers County. She is at home, quarantined and in stable condition. Her case may be travel-related.
Fort Bend County: 42 total cases, 4 recoveries
The total number of reported coronavirus cases in Fort Bend County is 42. Four recoveries have been reported.
Here is the information Fort Bend County health officials have provided about the cases:
- A man in his 70s who was hospitalized, released and now recovering at home.
- A woman in her 20s, with moderate symptoms and history of travel to a high incidence area, is recovering in isolation at home.
- A man in his 50s with moderate symptoms is recovering at home.
- A woman in her 50s with moderate symptoms is recovering at home.
- A woman in her 20s with moderate symptoms is recovering at home.
- A woman in her 20s with mild to moderate symptoms. She is recovering in isolation at home.
- A man in his 50s with mild to moderate symptoms. He is recovering in isolation at home.
- A man in his 60s who was hospitalized and discharged. He is now recovering in isolation at home.
- A woman in her 60s who is hospitalized.
- A woman in her 50s with mild to moderate symptoms. She is recovering in isolation at home.
- A woman in her 40s with international travel who has moderate symptoms and is in isolation at home.
- A woman in her 50s with domestic travel to a region with widespread local disease. She has moderate symptoms and is in isolation at home.
- A man in his 40s with domestic travel and mild to moderate symptoms. He is in isolation at home.
- A minor child with domestic travel and mild symptoms who is in isolation at home.
- A man in his 40s with domestic travel and moderate symptoms who is in isolation at home.
- A woman in her 30s with domestic travel and moderate symptoms who is in isolation at home.
- A man in his 30s with moderate symptoms who is recovering in isolation at home.
- A woman in her 70s with a history of international travel. She reported mild symptoms and is being isolated at home.
- A man in his 60s. He is hospitalized and in stable condition.
- A woman in her 20s who traveled internationally. She reported mild symptoms and is being isolated at her home.
- A man in his 40s, with a history of international travel and exposure to confirmed COVID-19 cases abroad. He experienced moderate flu-like symptoms, which have resolved. He is in isolation at home.
- A woman in her 50s, with a history of international travel. She experienced mild symptoms that have resolved. She is in isolation at home.
- A man in his 70s with a history of international travel. He was hospitalized and discharged in good condition. He is recovering in isolation at home.
- A man in his 70s in Fort Bend County is hospitalized and is in stable condition.
Galveston County: 18 total cases
The number of coronavirus cases that have been reported in Galveston County is at 18.
Here is the information Galveston County health officials have released thus far about the cases:
- A female younger than 10 years old with recent domestic travel. She is self-quarantined
- A male in his 20s with recent international travel. He is self-quarantined
- A male in his 50s with recent domestic travel. He is self-quarantined.
- A male in his 40s with recent domestic travel He is self-quarantined.
- A male in his 20s with recent international travel. He is self-quarantined.
- A male in his 60s with recent domestic travel. He is self-quarantined.
- A woman in her 40s, who recently traveled internationally and had contact with a positive coronavirus patient, is currently self-quarantined. She visited an area clinic.
- A man in his 70s who recently traveled domestically.
- A woman in her 20s believed to have been exposed through community spread.
- A woman in her 50s believed to have been exposed through community spread.
- A man in his 40s who recently traveled internationally. He is being isolated at home.
- A woman in her 50s who came in contact with a person known to have traveled to an area affected by coronavirus. She is being isolated at home.
- A man in his 50s who has recently traveled within the U.S. He is being isolated at home.
- A woman in her 40s who has recently traveled within the U.S. She is being isolated at home.
- A man between 45 and 50 years old who had symptoms that included fever, dry cough, sore throat, headaches and body aches.
- A woman between 30 to 35 years old who lives in northern Galveston County. Her case has been linked to a case in Montgomery County.
- A woman in her 30s, who recently traveled domestically. She visited a local urgent care facility and is currently self-quarantined.
- A woman in her 60s, who recently traveled domestically. She visited a local clinic and is self-quarantined.
Grimes County: 2 total cases
The total number of coronavirus cases reported in Grimes County is at 2.
Officials reported the first case in Grimes County on March 18 and said the second case was found in someone who lives with the person connected to the first case. Officials said neither of the infected people had any contact with anyone else in the county. Both are isolated at home, officials said.
Harris County: 54 total cases, 1 death, 12 recoveries
Harris County’s total number of reported coronavirus cases is 51. One death and 11 recoveries have been reported. This number does not include cases reported in the city of Houston. Those numbers are broken down in a separate entry below.
Here is the information Harris County health officials have provided about the cases thus far:
- A 40- to 49-year-old woman, who lives in the Northwest quadrant of Harris County- (recovered)
- A 60- 69-year-old woman, who lives in the Northwest quadrant of Harris County- (community spread)
- A 50- to 59-year-old man, who lives in the Northwest quadrant of Harris County- (travel-related)
- A 30- to 39-year-old woman, who lives in the northwest quadrant of Harris Count, exposed through community spread.
- A 50- to 59-year-old man, who lives in the northwest quadrant of Harris County, exposed by contact with a positive COVID-19 individual.
- A 40- to 49-year-old man, who lives in the northwest quadrant of Harris County, exposed through community spread.
- A 20- to 29-year-old man, who lives in the northwest quadrant of Harris County, exposed through community spread.
- A 40 to 49-year-old man, who lives in the southwest quadrant of Harris County, exposed through community spread.
- A 30- to 40-year-old man, who lives in the northwest quadrant of Harris County, exposed through a confirmed case.
- A 20- to 30-year-old woman, who lives in the northwest quadrant of Harris County, exposed through community spread.
- A 20- to 30-year-old man, who lives in the northwest quadrant of Harris County, exposure still pending investigation.
- A 30- to 40-year-old woman, who lives in the northwest quadrant of Harris County, exposed through to a confirmed case.
- A 0- to 10-year-old boy, who lives in the northwest quadrant of Harris County, exposed through a confirmed case.
- A 0- to 10-year-old girl, who lives in the northwest quadrant of Harris County, exposed through a confirmed case.
- A 10- to 20-year-old woman, who lives in the northwest quadrant of Harris County, exposed to a confirmed case.
- A 40- to 50-year-old woman, who lives in the northwest quadrant of Harris County, exposed through travel
- A 50- to 60-year-old man, who lives in the northeast quadrant of Harris County, exposure still pending investigation.
- A 50- to 60-year-old man, who lives in the northwest quadrant of Harris County, exposed through travel
- A 50- to 60-year-old woman, who lives in the northeast quadrant of Harris County- (community spread)
- A 20- to 30-year-old woman, who lives in the southwest quadrant of Harris County- (travel-related)
- A 40- to 50-year-old man, who lives in the southeast quadrant of Harris County- (investigation pending)
- A 20- to 30-year-old woman, who lives in northwest Harris County- (travel-related)
- A 30- to 40-year-old woman, who lives in northwest Harris County- (community spread)
- A 20- to 30-year-old woman, who lives in northwest Harris County- (community spread)
- A 50- to 60-year-old man, who lives in northwest Harris County- (community spread)
- A 50- to 60-year-old woman, who lives in the southeast Harris County- (community spread)
- A 40- to 50-year-old man, who lives in northwest Harris County- (travel-related)
- A 20- to 30-year-old woman, who lives in the southwest Harris County- (investigation pending)
- A 50- to 60-year-old man, who lives in the northwest Harris County- (travel-related)
- A 50- to 60-year-old woman, who lives in northeast Harris County- (investigation pending)
- A 40- to 50-year-old man who has no history of travel.
- A 30- to 40-year-old woman who lives in northeast Harris County. She had contact with a positive COVID-19 individual.
- A 30- to 40-year-old man who lives in northwest Harris County.
- An 80- to 90-year-old man who lived in a nursing home in northwest Harris County. His death was reported Thursday. This case was believed to be the result of community spread.
- A 20- to 30-year-old man who lives in northwest Harris County. This case is believed to be the result of community spread.
- A 40- to 50-year-old woman who lives in southwest Harris County. This case is believed to be the result of community spread.
- A 60- to 70-year-old man who lives in northeast Harris County and has not history of travel. This case is believed to be the result of community spread.
- A 30- to 40-year-old woman who lives in southwest Harris County and has no history of travel. This case is believed to be the result of community spread.
- A 40- to 50-year-old man who lives in northwest Harris County.
- A 40- to 50-year-old man who lives in northwest Harris County.
- A 40- to 50-year-old woman who lives in southwest Harris County.
- A 40- to 50-year-old woman who lives in northwest Harris County and is believed to have contact with a person who has COVID-19.
- A 50- to 60-year-old man who lives in northwest Harris County.
- A 40- to 50-year-old man in northwest Harris County.
- A 20- to 30-year-old woman who lives in southwest Harris county. She recently returned from Italy aboard two flights: Lufthansa 309 from Florence to Frankfurt on March 3 and United Airlines 47 from Frankfurt to Houston.
- A 60- to 70-year-old woman who lives in northwest Harris County. This case is believed to be travel-related.
- Three people between 60 and 70 years old and live in northwest Harris County.
- A man and a woman. The woman is a staff member of Rice University.
Houston: 24 total cases, 2 recoveries
The total number of reported coronavirus cases in the city of Houston is at 24.
Here is the information city health officials have provided about the cases thus far:
- A 20- to 30-year-old woman who has no known travel history. She is recovering at home.
- A 30- to 40-year-old-man who recently traveled to Idaho, who is at home recovering.
- A 60- to 70-year-old-woman with no known travel has been hospitalized.
- A 20- to 30-year-old man, who has traveled in Texas, is at home recovering.
- A 40- to 50-year-old man, who traveled to Costa Rica, is at home recovering.
- A 50- to 60-year-old woman who traveled to Kansas. She is hospitalized.
- A 40- to 50-year-old man who traveled to Georgia. He is hospitalized
- A 60- to 70-year-old woman with no travel history. She is at home, recovering
- A 50- to 60-year-old man who traveled to the UK. He is at home, recovering
- A 40- to 50-year-old man who traveled to New York, New Jersey and Pennsylvania. He is at home, recovering
- A 40- to 50-year-old man who traveled to Colorado. He is at home, recovering
- A 40- to 50-year-old man who traveled to Nevada. He is at home, recovering
- A 50- to 60-year-old woman with no history of travel or exposure to the coronavirus.
- A 50- to 60-year-old man with no history of travel.
- A 70- to 80-year-old man who traveled to New York.
- A 50- to 60-year-old man who traveled to Spain.
- A 20- to 30-year-old woman who traveled to Mexico.
- A 60- to 70-year-old man with no history of travel.
- A 70- to 80-year-old woman who traveled to Egypt.
- A 15- to 25-year-old female who traveled to New York.
- A 60- to 70-year-old man.
- A 60- to 70-year-old woman.
- A 50- to 60-year-old man with a history of international travel.
Liberty County: 1 total case
The total number of cases that have been reported in Liberty County is at 1.
Here is the information officials have released about the case thus far:
- A woman between 40 and 50 years old who is experiencing mild symptoms and isolated at home.
Matagorda County: 6 total cases, 1 death
The total number of coronavirus cases that have been reported in Matagorda County is at 6. One of those people died from the virus.
Here is the information officials have released thus far about the cases:
- A man between the ages of 55 and 65. Self-quarantining at home and in stable condition.
- A man between the ages of 18 and 25. Self-quarantining at home and in stable condition.
- A woman between 75 and 85 years old who had no travel outside of the county. She is at Matagorda Regional Medical Center in fair condition.
- A woman between 50 and 55 years old who recently traveled to Washington state.
- A man in his late 90s who died after suffering from symptoms consistent with COVID-19. A test conducted on him came back positive for coronavirus the day after he died.
- A 60-year-old woman who had been admitted to Matagorda Regional Medical Center for pneumonia complications and tested positive for coronavirus during a screening. She is “resting comfortably.”
Montgomery County: 19 total cases
The total number of coronavirus cases reported in Montgomery County is at 19.
Here is the information Montgomery County health officials have provided about the cases thus far:
- A man in his 50s, who resides in southwest Montgomery County. He is in isolation at his home. He recently traveled to California.
- A man in his 50s, who resides in southwest Montgomery County. He is in isolation at his home. He recently traveled to Chicago, Illinois
- A woman in her 20s, who lives in northwest Montgomery County. She is in isolation at her home. Believed to be a case of community spread.
- A female teen between 13 and 19 years old, who lives in southeast Montgomery County. She is in isolation at home. She recently traveled to New Orleans
- A woman in her 40s, who lives in southwest Montgomery County, is connected to a case in Smith County, where she recently traveled. She is at home in isolation.
- A man is in his 40s, who has been in northeast Montgomery County for work-related purposes, is at home in isolation. His only recent travel is to Houston.
- A man in his 90s, who lives in southwest Montgomery County. He is currently hospitalized. He has no recent travel history
- A man in his 50s, who lives in southwest Montgomery County. His case is still under investigation.
- A woman in her 50s who lives in southeast Montgomery County. She is in isolation at home and she attended the Houston Rodeo on March 8.
- A man in his 50s who lives in southwest Montgomery County. He is hospitalized in critical but stable condition.
- A woman in her 40s who lives in southeast Montgomery County. She recently traveled to Germany. She is being kept in isolation at her home.
- A woman in her 60s who lives in northwest Montgomery County who has no recent history of travel.
- A man in his 40s who lives in southwest Montgomery County. He recently traveled to California. He is being kept in isolation at his home.
- A man in his 50s who lives in south Montgomery County and recently traveled to California. He is being kept in isolation at his home.
- A woman in her 40s who lives in northwest Montgomery County. She is being kept in isolation at her home.
- A man in his 40s who lives in northwest Montgomery County and recently traveled to Florida.
- A woman in her 40s who lives in south Montgomery County and recently traveled to New Orleans. She is being treated at an area hospital.
- A man in his 40s who lives in northwest Montgomery County. He is being treated at an area hospital.
- A woman in her 30s, who resides in northwest Montgomery County. She is in isolation at home and has no recent travel history.
Walker County: 1 total case
The total number of cases that have been reported in Walker County is at 1.
The patient is male, in his 20s, and the source of the exposure is still under investigation. The person was tested outside of Walker County. He is experiencing mild symptoms and has been isolated at home.
Wharton County: 1 total case
The total number of coronavirus cases reported in Wharton County is 1.
More of our coronavirus coverage
FIND ALL OF OUR COVERAGE: See everything you need to know about coronavirus on our special page.
LOCAL CASES: See all the latest local coronavirus updates in our blog
TOTAL CASES: Keep track as new coronavirus cases are reported in counties in the Houston area
TEXAS: Here’s everything you need to know about the coronavirus in Texas
MAPPED: See a Johns Hopkins interactive map that shows how coronavirus has spread through the world
DEATHS: Here’s what we know about the 100 people who’ve died in the US from coronavirus
March 23, 2020
Coronavirus in Texas
Coronavirus in Texas: At least 325 cases reported in state; Abbott moves to bolster number of practicing nurses
:strip_exif(true):strip_icc(true):no_upscale(true):quality(65)/arc-anglerfish-arc2-prod-gmg.s3.amazonaws.com/public/Z5XBERHGA5EQNC3JV4IP2PXC3Q.jpg)
The most affected county is Dallas, with 29 cases, followed by Harris, with 25. Travis and Bexar counties follow with 22 each. The statewide numbers for specific counties are lagging local media reports and may differ from what local officials have disclosed. Generally, counties are reporting how many patients test positive there. The state classifies people with positives tests by the county they live in, regardless of where they got tested or are being treated.
The state reported 83 cases where investigators are still determining the county of residence. At least 6,522 tests have been administered, a 414% increase over Tuesday’s testing total of 1,268 when the state first released testing numbers. — Carla Astudillo
Abbott hoping to increase number of practicing nurses, waives some licensing rules
[1:04 p.m.] Gov. Greg Abbott announced Saturday he would waive certain regulations to allow nursing students and retired nurses to easily join the workforce, as the need for medical professionals grows during the novel coronavirus crisis.He said the state would allow graduate nurses and vocational nurses who haven’t yet taken the licensing exam to receive temporary permit extensions allowing them to practice. Students in their final year of nursing school can more easily meet clinical requirements. And nurses with inactive licenses and retired nurses can reactive their licenses.
“Nurses are essential to our ability to test for this virus, provide care for COVID-19 patients, and to continue providing other essential health care services. Suspending these regulations will allow us to bring additional skilled nurses into the workforce to assist with our efforts and enhance our COVID-19 response,” he said in the release. — Aliyya Swaby
May primary runoff elections delayed until July
The May 26 primary election runoffs will be delayed until July in response to the growing outbreak of the new coronavirus in Texas under an order signed Friday by Gov. Greg Abbott.
Abbott signed the postponement under the emergency powers of his previous statewide disaster declaration. The elections are now scheduled for July 14; early voting will begin July 6.
Before Abbott’s announcement, Texas Democrats instead turned to the state courts Friday to push for expanding mail-in voting. — Alexa Ura
Health care providers delay non-urgent appointments, surgeries
[6:54 p.m.] In an effort to protect their staff and patients from COVID-19 during a time when people are being encouraged to stay 6 feet away from each other, health care providers across the state have postponed check-ups, elective surgeries and other non-urgent medical appointments that must be conducted in person. Likewise, some patients who need regular medical care are putting it off, afraid of contracting the virus in crowded waiting rooms or from health care workers who may not have access to adequate personal protective equipment.But there are certain procedures and other in-person visits that can only be delayed so long. That has patients and health care providers alike asking the same question: How long is the coronavirus pandemic going to last and demand social isolation?
“We don’t know, and there’s no one who can tell you,” said Dr. Jim McDeavitt, senior vice president of operations and dean of clinical affairs at Baylor College of Medicine in Houston. As with the economy, education and beyond, “the longer this goes on, the more challenging it’s going to get.” — Kiah Collier
Texas small businesses can apply for emergency federal loans
[6:54 p.m.] Small businesses battered by the novel coronavirus pandemic sweeping through Texas can apply for long-term, low-interest loans from the U.S. Small Business Administration, Gov. Greg Abbott announced Friday. The Economic Injury Disaster Loan is available for small businesses to apply. Questions of eligibility, and how to apply, can be answered on the agency website. — Mitchell FermanTroubled restaurants want sales tax payment delay, but state needs that money to respond to the virus
[2:46 p.m.] Texas restaurant owners say they could ride out the new coronavirus’ social slowdown for months if the state waived, delayed or deferred Friday’s deadline to pay sales taxes from last month. But Comptroller Glenn Hegar said the state won’t push back the deadline because, most importantly, the state and local governments that depend on those taxes to keep hospitals and emergency services going need the money as they prepare for the number of Texans testing positive to skyrocket within weeks. — Mitchell Ferman and Ross RamseyMore than 200 people have tested positive for the coronavirus in Texas
[12:45 p.m.] In Texas, at least 212 people have tested positive for the novel coronavirus, and five people have died, according to the latest numbers provided Thursday by the Texas Department of State Health Services and the Centers for Disease Control and Prevention. This is 30% more than the 161 cases reported Thursday and an 123% increase from the 95 cases reported Wednesday. The most affected county is Harris, with 24 cases, followed by Dallas, with 22. Travis follows with 21. The state tracks cases by county of residence, and some patients are treated outside of the county where they live, so today’s data also lists 19 cases in which investigators are still determining the county of residence.The state health agency says that these numbers may differ from local reports, given that some jurisdictions are making their data public before sending it to the state and also because they might be including residents of other counties in their reports. At least 5,277 tests have been administered, a 125% increase over yesterday’s testing total. — Darla Cameron
Abbott suspends prisoner health care fees
[12 p.m.] Gov. Greg Abbott directed the Texas prison system to temporarily suspend prisoner health care fees for services related to COVID-19 to “encourage timely reporting of COVID-19 symptoms so that offenders are given the treatment they need,” according to a news release from the governor’s office.As of September, prisoner health care costs were $13.55 per medical visit, with an annual cap of $100 a year. Prison reform advocates have argued that higher fees dissuade inmates from seeking treatment.
“Waiving health care fees for offenders housed in [Texas Department of Criminal Justice] facilities will ensure that inmates experiencing any symptoms of COVID-19 receive immediate medical attention,” Abbott said in the release. “This suspension will protect the health of both inmates and TDCJ staff, and is a crucial tool in our efforts to mitigate any potential spread of COVID-19 in closely confined populations.”
TDCJ holds about 140,000 inmates in its more than 100 prison facilities. The department has not yet reported any cases of the new coronavirus, though testing is only being performed by outside entities if an inmate has been taken to a hospital and a doctor there orders it, according to a prison spokesperson. — Jolie McCullough
Calls increase for Trump administration to release migrants from detention
[5 a.m.] As the new coronavirus infects more than 11,000 Americans, including more than 160 Texans so far, immigrant rights groups and attorneys are calling for the government to release detained migrants before the pandemic creates an irreversible health crisis inside detention facilities.“A number of detainees in recent days have told us how frightened they are to be locked in detention as the coronavirus spreads throughout the country,” the Refugee and Immigrant Center for Education and Legal Services said in a statement. “We demand that ICE release all immigrant detainees immediately.”
The Immigration and Customs Enforcement website details its procedures, including isolation, in the event that a detained person gets COVID-19, the disease caused by the new coronavirus. But more than 750 private entities wrote to ICE acting Director Matthew T. Albence on Thursday arguing that the agency’s track record under the Trump administration does nothing to instill confidence that detainees are being kept in safe environments. — Julián Aguilar
Copyright 2020 by KPRC Click2Houston – All rights reserved.
Manage Anxiety & Stress
Español On This Page
- Reducing stress in yourself and others
- Information for parents
- Information for responders
- Information for people released from quarantine
Stress and Coping
The outbreak of coronavirus disease 2019 (COVID-19) may be stressful for people. Fear and anxiety about a disease can be overwhelming and cause strong emotions in adults and children. Coping with stress will make you, the people you care about, and your community stronger.
Everyone reacts differently to stressful situations. How you respond to the outbreak can depend on your background, the things that make you different from other people, and the community you live in.
People who may respond more strongly to the stress of a crisis include
- Older people and people with chronic diseases who are at higher risk for COVID-19
- Children and teens
- People who are helping with the response to COVID-19, like doctors and other health care providers, or first responders
- People who have mental health conditions including problems with substance use
If you, or someone you care about, are feeling overwhelmed with emotions like sadness, depression, or anxiety, or feel like you want to harm yourself or others call
- 911
- Substance Abuse and Mental Health Services Administration’s (SAMHSA’s) Disaster Distress Helpline: 1-800-985-5990 or text TalkWithUs to 66746. (TTY 1-800-846-8517)
Stress during an infectious disease outbreak can include
- Fear and worry about your own health and the health of your loved ones
- Changes in sleep or eating patterns
- Difficulty sleeping or concentrating
- Worsening of chronic health problems
- Increased use of alcohol, tobacco, or other drugs
People with preexisting mental health conditions should continue with their treatment and be aware of new or worsening symptoms. Additional information can be found at the Substance Abuse and Mental Health Services Administration (SAMHSAexternal icon) website.
Taking care of yourself, your friends, and your family can help you cope with stress. Helping others cope with their stress can also make your community stronger.
Things you can do to support yourself
- Take breaks from watching, reading, or listening to news stories, including social media. Hearing about the pandemic repeatedly can be upsetting.
- Take care of your body. Take deep breaths, stretch, or meditate. Try to eat healthy, well-balanced meals, exercise regularly, get plenty of sleep, and avoid alcohol and drugs.
- Make time to unwind. Try to do some other activities you enjoy.
- Connect with others. Talk with people you trust about your concerns and how you are feeling.
Call your healthcare provider if stress gets in the way of your daily activities for several days in a row.
Reduce stress in yourself and others
Sharing the facts about COVID-19 and understanding the actual risk to yourself and people you care about can make an outbreak less stressful..
When you share accurate information about COVID-19 you can help make people feel less stressed and allow you to connect with them.
Learn more about taking care of your emotional health.
For parents
Children and teens react, in part, on what they see from the adults around them. When parents and caregivers deal with the COVID-19 calmly and confidently, they can provide the best support for their children. Parents can be more reassuring to others around them, especially children, if they are better prepared.
Not all children and teens respond to stress in the same way. Some common changes to watch for include
- Excessive crying or irritation in younger children
- Returning to behaviors they have outgrown (for example, toileting accidents or bedwetting)
- Excessive worry or sadness
- Unhealthy eating or sleeping habits
- Irritability and “acting out” behaviors in teens
- Poor school performance or avoiding school
- Difficulty with attention and concentration
- Avoidance of activities enjoyed in the past
- Unexplained headaches or body pain
- Use of alcohol, tobacco, or other drugs
There are many things you can do to support your child
- Take time to talk with your child or teen about the COVID-19 outbreak. Answer questions and share facts about COVID-19 in a way that your child or teen can understand.
- Reassure your child or teen that they are safe. Let them know it is ok if they feel upset. Share with them how you deal with your own stress so that they can learn how to cope from you.
- Limit your family’s exposure to news coverage of the event, including social media. Children may misinterpret what they hear and can be frightened about something they do not understand.
- Try to keep up with regular routines. If schools are closed, create a schedule for learning activities and relaxing or fun activities.
- Be a role model. Take breaks, get plenty of sleep, exercise, and eat well. Connect with your friends and family members.
Learn more about helping children cope.
For responders
Responding to COVID-19 can take an emotional toll on you. There are things you can do to reduce secondary traumatic stress (STS) reactions:
- Acknowledge that STS can impact anyone helping families after a traumatic event.
- Learn the symptoms including physical (fatigue, illness) and mental (fear, withdrawal, guilt).
- Allow time for you and your family to recover from responding to the pandemic.
- Create a menu of personal self-care activities that you enjoy, such as spending time with friends and family, exercising, or reading a book.
- Take a break from media coverage of COVID-19.
- Ask for help if you feel overwhelmed or concerned that COVID-19 is affecting your ability to care for your family and patients as you did before the outbreak.
Learn more tips for taking care of yourself during emergency response.
For people who have been released from quarantine
Being separated from others if a healthcare provider thinks you may have been exposed to COVID-19 can be stressful, even if you do not get sick. Everyone feels differently after coming out of quarantine. Some feelings include :
- Mixed emotions, including relief after quarantine
- Fear and worry about your own health and the health of your loved ones
- Stress from the experience of monitoring yourself or being monitored by others for signs and symptoms of COVID-19
- Sadness, anger, or frustration because friends or loved ones have unfounded fears of contracting the disease from contact with you, even though you have been determined not to be contagious
- Guilt about not being able to perform normal work or parenting duties during quarantine
- Other emotional or mental health changes
Children may also feel upset or have other strong emotions if they, or someone they know, has been released from quarantine. You can help your child cope. Resources
For Everyone
For Communities
- Coping with stress during an infectious disease outbreakpdf iconexternal icon
- Taking Care of Your Behavioral Health during an Infectious Disease Outbreakexternal icon
For Families and Children
- Helping Children Cope with Emergencies
- Coping After a Disasterpdf icon – A Ready Wrigley activity book for children age 3-10
For First Responders
- Emergency Responders: Tips for taking care of yourself
- Disaster Technical Assistance Centerexternal icon (SAMHSA)
March 22, 2020 David Ho; Virologist
As of March 20, more than 8,700 people worldwide had died of COVID-19, the disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Caltech trustee David Ho (BS ’74) of the Aaron Diamond AIDS Research Center, Columbia University, says that this is just the tip of the iceberg. Ho, an expert on viral epidemics, has spent decades researching HIV/AIDS, having begun his career in Los Angeles, “ground zero” of the first outbreak, in the early 1980s. On March 18, Ho sat down with members of the Caltech community to discuss the novel coronavirus and the future of our society in the light of this global pandemic.
Walk us through the spread of the virus in the United States. What does the country look like right now?
Let me just give you a picture of what I see here in New York. About two weeks ago, we had our initial case, and now in New York City newly diagnosed confirmed cases are tripling every two days. In our New York Presbyterian Hospital, approximately 25 percent of the swab samples that are submitted for testing are positive. In the suburban communities outside of New York, approximately 10 percent of the swabs submitted are positive. So, the virus is everywhere. And in New York, we know that we are in the exponential growth phase of the epidemic.
Looking back at what has transpired throughout the world, we saw the first wave hit China; the second wave hit South Korea, Italy, and Iran; and then, trailed by only about a week or so, France, Germany, Spain, and the U.S. We all know that China went through a period of great devastation. It has over 80,000 cases. Italy is rapidly catching up, with over 31,000 cases. We suspect that in the U.S. this will rapidly sweep from the coastal regions and it will hit middle America. It is already there, but we will see exponential growth very, very soon. Then of course we are all worried about what would happen when this epidemic strikes places like Africa and India where the health care system is less developed.
Can you tell us about the pathology of the disease?
COVID-19 typically causes fever and a dry cough. One may have aches in the body—the muscles—and if it’s severe enough, there would be shortness of breath due to pneumonia.
Gastrointestinal symptoms can occur and are an indication of more severe disease. It’s not very common to have a runny nose or the sniffles, and a sore throat is not common either.
The incubation period from exposure to onset of symptoms is between four and six days; and if you want to cover 95–98 percent of the cases it is between three and 10 days. It’s pretty rare to have an incubation period outside of that range.
What in particular makes this virus so dangerous?
What is disturbing is that virus shedding, as detected in the mouth or nose, is very, very common and could be there prior to onset of symptoms. That’s why transmission could occur from asymptomatic individuals. And virus shedding could continue for days up to three weeks after a person recovers. That is extremely worrisome for the spread of this virus. Furthermore, the stability of this virus is worrisome as well. If you put it in aerosol form and keep it in the air, the half-life is several hours; if you drop it on surfaces of copper or cardboard, it could survive about a day. But if it’s on steel or plastic surfaces, you could still detect infectious virus after 72 hours, although the infectivity decreases with time.
What do we know about the biology of the virus?
The virus is highly related to another coronavirus called SARS coronavirus. That was another outbreak that occurred worldwide 17-18 years ago, and largely in China and Asia.
The two viruses are about 80 percent identical. We know the origin of SARS was from a bat through an intermediary animal called the civet cat.
Another virus called Middle Eastern Respiratory Virus, MERS, also originated in bats and infected camels, and camels passed it to humans. For COVID-19, we believe the original host must be a bat species, because that animal carries a virus that’s 97 percent identical to what we’re seeing now.
Because of the SARS outbreak and the MERS outbreak, and research done on those two pathogens, we actually know quite a bit about coronaviruses.
The outbreak began in China; how have they been dealing with the virus?
This epidemic was first identified in a few cases with pneumonia in December 2019. In retrospect, there were scattered cases in November according to Chinese officials. I would say that initially there were missteps and lack of transparency that contributed to the explosive outbreak in the city of Wuhan in the central province of Hubei. That epidemic in central China accounts for 85 percent of the confirmed cases in China. It led Beijing officials to quarantine the entire province of 50 million people. The epidemic peaked in early February with 4,000 newly diagnosed cases each day. But since the lockdown and the various draconian measures applied, the number of new cases each day has been declining by half every week, and remarkably it’s now down to about 20 per day. The rest of China’s other provinces also applied very harsh measures and they indeed successfully flattened the curve outside of Hubei province.
We know what they’ve done is not sustainable and the question is: What is China going to do now if it relaxes the infection control measures? Some of the recovered patients are still shedding virus and now China is surrounded by sick neighbors. Surely if they open up their borders, infection will come in the same way it came into the U.S. The world is waiting to see what China is going to do.
Now in terms of the U.S., we obviously are undergoing exponential growth. The 10,400 confirmed cases is a gross underestimate. The lack of testing is embarrassing. It’s an outright failure in leadership.
What are the tests we need to detect coronavirus infection?
Everybody’s talking about testing and that’s actually referring to PCR [polymerase chain reaction] testing, looking for viral RNA to determine whether a person is infected. But there’s still no talk of antibody testing to determine which people have had it and are immune, and that is another crucial tool we need to combat this epidemic. Many research labs throughout the country—I’m sure at Caltech too—could be running antibody tests right now to survey the population and tell us what the real penetrance of this pathogen is in our communities. We are, on a research basis, embarking on that to understand the degree of infection in New York City and outside of New York City.
How long before the U.S. sees test availability similar to what South Korea has implemented?
The PCR testing, which is the one that’s approved, is now ramping up very, very rapidly in state and local labs as well as in academic medical centers and in the commercial sector. Their production will grow tremendously. Roche has a machine that will run 1,000 samples at a time. If you go to a commercial lab, they take a swab, they package it, they quite often send it to another facility somewhere else. The turnaround time is typically 72 hours. In that period, it’s very, very hard to manage patients and their contacts. It’s a nightmare for the healthcare worker.
We need point-of-care tests. Those kinds of tests are available for HIV and for many other diseases; you use a finger stick, drop the blood on a small device, and have a readout in 15 minutes. These tests measure antibody response to the virus and are extremely useful. Yet we don’t have a single test licensed in the U.S. In China, in South Korea, and in Europe, those tests are used. The manufacturer for this rapid test is producing a million a day. It’s there. But in the name of protecting the public, the FDA has moved very, very slowly. That delay, in my view, has caused more harm than good.
Can you elaborate on point-of-care testing?
It’s almost like a home pregnancy test or home HIV test. These tests have been around for a long time. The test that I’m specifically referring to, coming out of China, South Korea, and approved in Europe, is an antibody test. You put a drop of blood on a plastic slide, add another drop of the buffer that comes with the test, and you let it sit for 15 minutes. Then, you look at the bands. You’re negative if you have just one band, or you’re positive if you have more than one band. The test also tells you type of antibody. There’s a type of antibody called IgG [immunoglobulin G] and another type called IgM [immunoglobulin M]. Typically, when a person is infected, the IgM response is earlier and the IgG response is later. The two bands indicate the course of the infection.
This kind of test is available all over the world for HIV. The technology is there, the tests are there. But they’re not FDA approved. While I think they are fairly close to being approved, we have let several weeks go by and to me that’s tragic.
Will this coronavirus be seasonal?
Everyone is asking whether this virus is here to stay. Initially, just based on what China did with SARS long ago, there was hope that warmer weather and more sunlight would help kill the virus in our environment and therefore lower the probability of transmission.
But now this virus has gained such a strong foothold in the human population. It’s already 25 times larger than SARS and it’s already embedded in the Southern hemisphere. If you look at Australia, South Africa, Argentina, Brazil, there are cases there already, and community transmission is occurring. As the weather changes, perhaps the Northern hemisphere will gain an advantage. But the epidemic in the Southern hemisphere is going to accelerate.
The long-term outcome may resemble influenza so that we have seasonal bouts, with the virus bouncing back and forth between the Northern and Southern hemispheres. This is of course just speculation, but that’s what we see with influenza.
Why does COVID-19 have less impact on children and more impact on the elderly?
Well, the latter part is easy. Older people generally do less well with all sorts of respiratory infections, including influenza and SARS. So that’s just the typical scenario we see. The children, however, are a mystery. As you know, children typically get flu or other respiratory viruses very quickly and bring them home to infect the parents. But in this particular case, the number of children infected in China, after extensive studies, don’t seem to indicate that this is the case for this coronavirus.
Some people seem to show mild symptoms while others have a more severe experience. Has the virus already mutated?
RNA viruses all replicate with low fidelity. Mutations occur at pretty similar rates and these viruses typically don’t have proofreading functions. In contrast, we replicate our DNA with high fidelity and we have a proofreading function to fix the errors. So, every time they replicate, there’s a fixed rate of mutation. This virus is mutating but it has mutated very little so far. There are differences but probably they are functionally not important, so that’s not the explanation for why you see different disease courses among the infected.
For HIV it’s the same thing: 10 people could be infected by the same strain but you have very different outcomes. With HIV, genetics and environmental factors play a role. Some of the genetics has been worked out; we know that there are certain tissue types that would protect and others that would harm. I suspect it’s the same here.
Once you become infected with the virus, can you get it again?
There are a few anecdotes from China about re-infection but, if you look at those reports carefully, they’re not well-documented. It could be that folks just continued to shed virus from the initial infection. Only one study was formally done and it is not a human study. It’s a macaque study. They infected macaques with this virus, then waited until the monkeys recovered and tried to re-infect them. They could not. This just came out in the past few days. That bodes well for human immunity.
We have now looked at a lot of serum from convalescent individuals and those serum samples have antibodies against the so-called spike protein of the virus. That’s the protein that sits on the surface of the virus particle. By tightly binding, the antibody could neutralize the virus. Once an infected person develops antibodies, there should be protective immunity for quite some time. That’s why we need to buy time for immunity to develop in the population.
After a person recovers from the virus, how long are they still contagious?
That’s a very important question. We’re not sure; one individual in China was shown to have persistent virus shedding for over a month. But typically, we’re looking at a three-week period from onset of symptoms.
What should we be doing to limit the spread of this epidemic?
The social distancing and good hygiene strategies have been successfully applied, in South Korea for example, to bring their epidemic down. They’re the only other country that has flattened the curve—slowed down the number of new infections to not overwhelm the healthcare system—and gradually brought this epidemic under control. There are many places that have done a pretty good job of not allowing the epidemic to explode, such as Taiwan and Hong Kong. These are places that had quite a bit of experience in fighting SARS, 17 years ago.
Are you optimistic that these measures combined with research will be enough to combat the coronavirus?
I personally believe we will blunt this epidemic, but I think we wasted a good four to six weeks largely because of lack of testing and lack of a certain preparedness. But I think we could still make a difference and bring it under control with very harsh measures.
But again, are these measures sustainable? We’ve got to expect that businesses must reopen and schools must teach again. Whether it’s travel or sports or live entertainment, we’re going to have to return to some semblance of normalcy. But what are the measures that are effective and sustainable? That’s a question we as a society have to deal with. We need to buy time so that gradually the population will have a degree of immunity.
Most importantly, we need to buy time to allow science to deliver solutions. We’re going to have to develop drugs, antibodies, and vaccines. I think the mobilization by the scientific community, from my perspective, is amazing. So many people have mobilized and jumped on this and are contributing, from discovering small-molecule drugs that could block various enzymes of this virus to coming up with antibodies that could neutralize the virus. Researchers have already come up with a few promising chemicals that could be a good start to drug development. There are already a few neutralizing antibodies isolated from infected individuals; my own group is in the midst of doing all that.
And, of course, people are working on vaccines. A lot of companies are working on vaccines and those vaccines are at various stages. A couple are within weeks of entering human testing and that’s quite, quite remarkable. There is one thing about vaccines, though: Some of the experiments previously done on SARS suggested that when animals developed antibodies and then were given the virus, they had greater lung injury due to the presence of the antibodies. The scientific community would have to resolve that issue quickly and its resolution would either halt the current approaches or unleash them to move full speed ahead. We certainly will take a part in doing that. I think we have the real possibility that COVID-19 may become a fact of life until science comes through as it has done for past epidemics.
This is going to take some time. But I’m very confident that the science will rise to the task and provide a solution. But it’s not going to be a few months as our president suggests. It’s going to be much longer than that. I would say 18 months, or 24 months. I think we are all facing tough challenges ahead.
March 21, 2020
The US government is reportedly preparing for the coronavirus pandemic to last 18 months or longer and result in “significant shortages for government, private sector, and individual US consumers.”
A 100-page US government plan was leaked to The New York Times, which today published an article summarizing the highlights.
“A federal government plan to combat the coronavirus warned policymakers last week that a pandemic ‘will last 18 months or longer’ and could include ‘multiple waves,’ resulting in widespread shortages that would strain consumers and the nation’s health care system,” the Times wrote.
The 18-month figure is in line with the best-case estimates of how long it will take to develop a vaccine and make it widely available. There could be millions of deaths in the US and UK alone during that time, but social distancing and other containment measures could limit the death toll, according to Imperial College London research that we wrote about yesterday.
The Times did not publish the full US government report. “Much of the plan is bureaucratic in nature, describing coordination among agencies and actions that in some cases have already been taken, like urging schools to close and large events to be canceled,” the article said.
The plan’s warnings include the following:
Shortages of products may occur, impacting health care, emergency services, and other elements of critical infrastructure… This includes potentially critical shortages of diagnostics, medical supplies (including PPE [personal protective equipment] and pharmaceuticals), and staffing in some locations.
State and local governments, as well as critical infrastructure and communications channels, will be stressed and potentially less reliable. These stresses may also increase the challenges of getting updated messages and coordinating guidance to these jurisdictions directly.
The Times article said the plan listed actions President Trump could take, such as “invoking the Defense Production Act of 1950, a Korean War-era law that authorizes a president to take extraordinary action to force American industry to ramp up production of critical equipment and supplies such as ventilators, respirators and protective gear for health care workers.”
Trump said on Tuesday that “we hope we don’t need” to invoke the Defense Production Act but that “we’ll make that decision pretty quickly if we need it,” the Times wrote.
Other options for the US mentioned in the government plan “include distributing medical supplies and equipment from the Strategic National Stockpile, providing money to states to help them meet demands caused by the coronavirus outbreak and prioritizing the distribution of essential resources to focus on areas most in need,” the Times wrote.
Update at 12:53pm ET: Trump announced today that he will invoke the Defense Production Act “just in case we need it.”
https://en.wikipedia.org/wiki/Hydroxychloroquine
https://www.foxnews.com/health/early-symptom-coronavirus-might-be-digestive-issues-study
https://abc13.com/health/7-people-recover-from-coronavirus-in-houston-area-officials-say-/5999764/
March 20, 2020 https://en.wikipedia.org/wiki/Hydroxychloroquine
March 20, 2020 https://www.foxnews.com/health/early-symptom-coronavirus-might-be-digestive-issues-study
Hello everyone, the Texas Department of Health has released some helpful graphics in order to distribute information in our community about the most frequently asked questions and what you can do right now. First we have what to do:
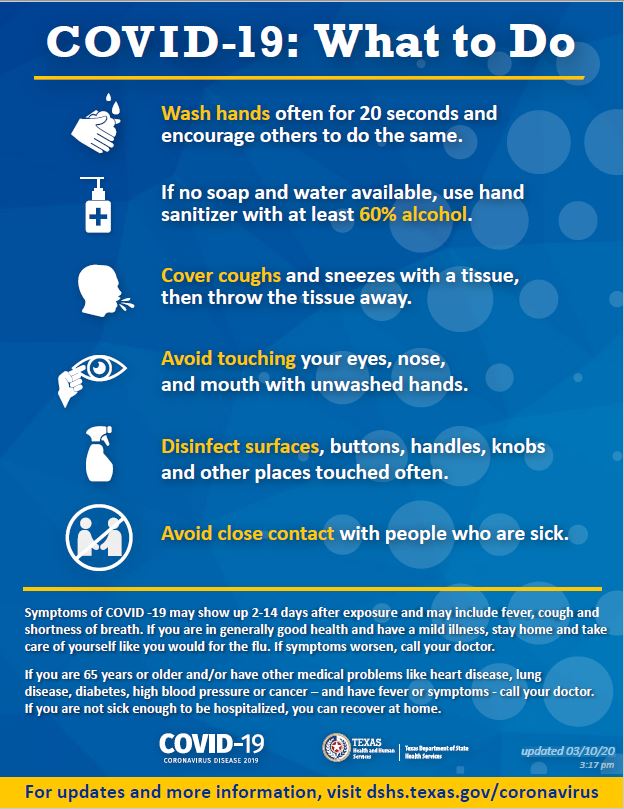
Next we have a collection of facts about the virus:
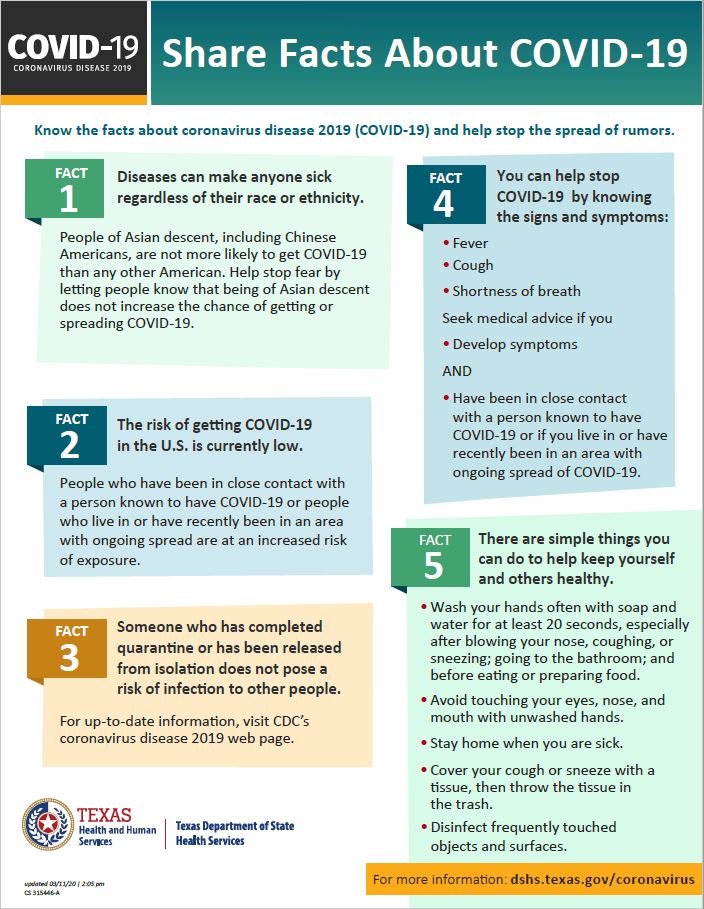
Tips for stopping the spread of the disease:

Finally, an alert to companies about the virus and what steps they should take:
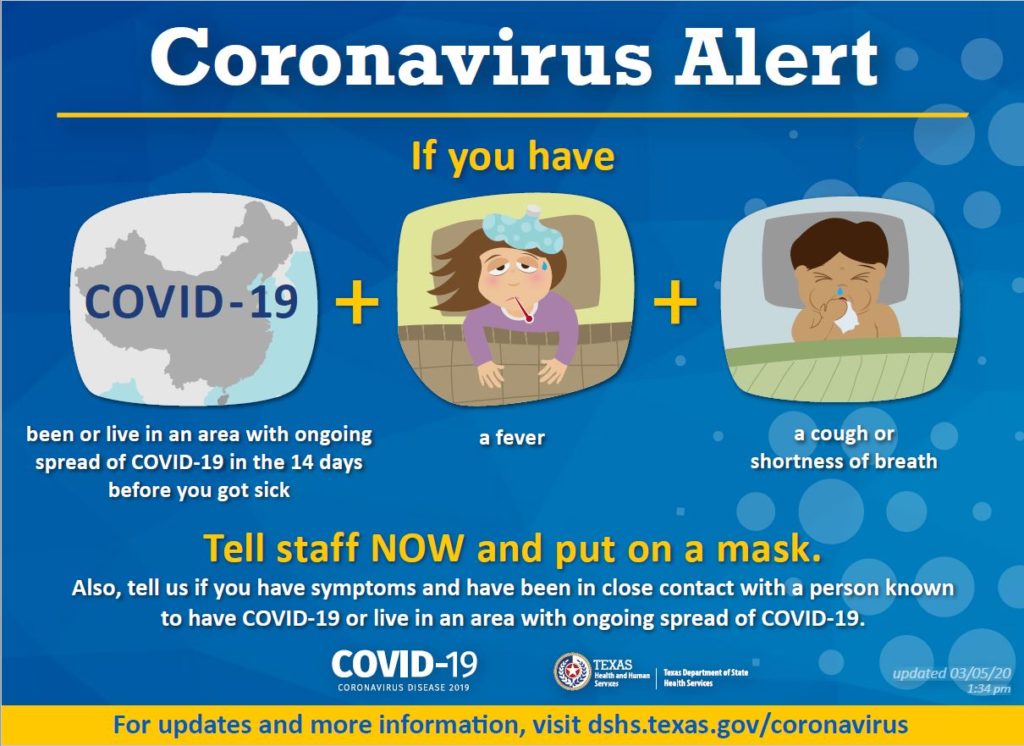
Thank you for reading through the graphics and becoming informed on the global threat that we face. These guidelines will help more people stay healthy and slow the spread of the Coronavirus.
FILED UNDER: Home Healthcare
